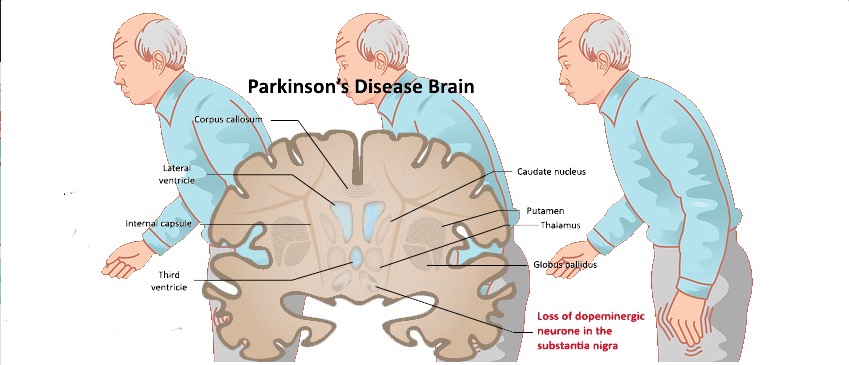
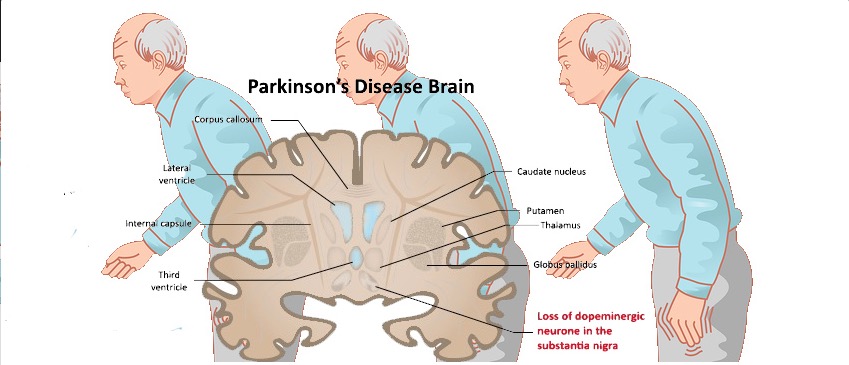
帕金森病(PD)是最常见的神经退行性疾病之一,但其发病机制仍不清楚。
目前的证据表明,神经炎症是帕金森病神经退行性疾病的病因和进展的一个主要因素。神经炎症不是对神经变性的简单反应,PD与中枢和外周的免疫反应都有关。
有证据表明,在PD中存在着脑-外周的相互作用,或者是通过胶质-淋巴途径,或者是通过血脑屏障的干扰。
据描述,与健康对照组(HCs)相比,PD患者的血液、脑脊液(CSF)和大脑中的促炎症细胞因子升高了。
在PD患者的外周血中,白细胞及其亚群的数量和质量都发生了变化。中性粒细胞与淋巴细胞比率(neutrophil-to-lymphocyte ratio,NLR)是一个公认的机体整体炎症状态的指标。
该比率整合了两种白细胞亚群和互补的免疫途径的信息:中性粒细胞与慢性炎症有关,而淋巴细胞可能代表调节途径。它已被用作癌症、心血管和炎症性疾病的预后因素,以及阿尔茨海默病的认知障碍的标志物。有人认为NLR在PD中升高,作为外周炎症的生物标志物,但结果有争议。
藉此,西班牙Universitario Virgen del Rocío的Laura Muñoz-Delgado等人,探究了PD患者与HCs相比,是否存在促炎症的外周免疫状态。
他们首先通过病例对照研究探究了PD患者和HCs之间外周免疫状况的差异。
然后,探究了NLR是否与PD的临床特征有关。
最后,进行了荟萃分析以澄清NLR在PD中的作用。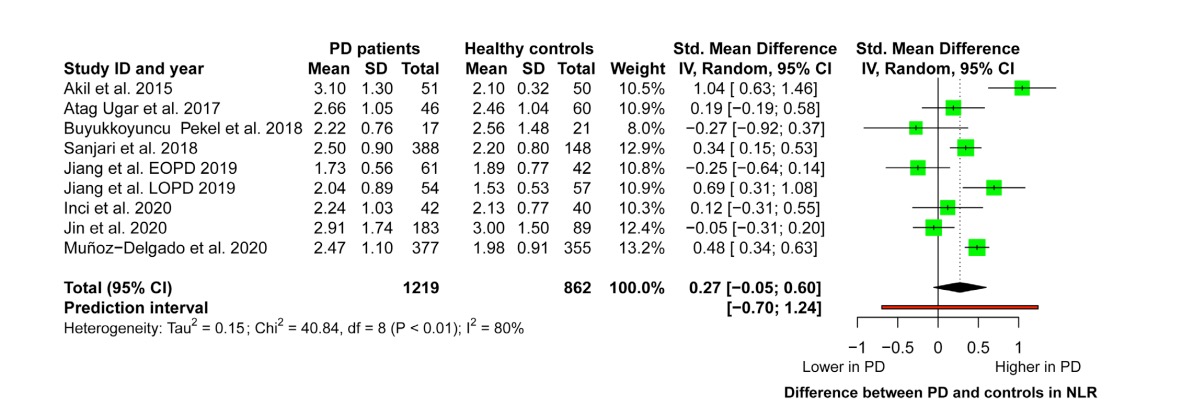
他们发现:在病例对照研究中,PD患者的NLR明显高于HCs(2.47 ± 1.1 vs. 1.98 ± 0.91,P < 0.001)。
但没有发现NLR与发病年龄、疾病严重程度或疾病持续时间之间的关联。
荟萃分析显示,PD患者的NLR可能更高。
这个研究的重要意义在于发现了:与HCs相比,PD患者的外周免疫谱发生改变,NLR较高。
原文出处:
Peripheral Immune Profile and Neutrophil‐to‐Lymphocyte Ratio in Parkinson’s Disease. Mov Disord. Published online June 8, 2021:mds.28685. doi:10.1002/mds.28685
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















#Disord#
70
#Dis#
81
#免疫特征#
81
#外周血#
90
有收获
95
学习了
79
顶
99