Blood:诱导缓解早期MRD水平对ALL患儿采用低强度化疗预后的影响
2020-10-12 星云 MedSci原创
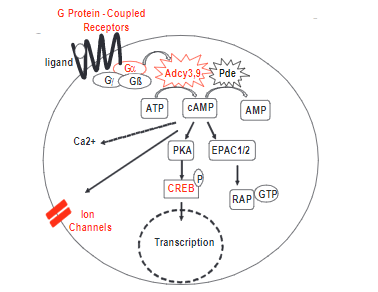
既往数据显示,大约40%的急性淋巴细胞白血病(ALL)患儿通过限制性的基于抗代谢药物的化疗方案治愈。然而,目前仍不能准确地鉴别具有极低风险(VLR)的患者。
既往数据显示,大约40%的急性淋巴细胞白血病(ALL)患儿通过限制性的基于抗代谢药物的化疗方案治愈。然而,目前仍不能准确地鉴别具有极低风险(VLR)的患者。
根据诱导性治疗第19天出现的症状和最小残留病(MRD)水平<0.01%相结合选择的患者经低强度的治疗可获得较好的预后。
在本研究中,Sidhom等调查了诱导缓解早期,MRD水平在0.001%~<0.01%之间对采用低强度方案治疗的VLR ALL患者预后的影响。
自2011年10月至2015年9月,共200例B-前体ALL患者具有良好临床病理特征,在诱导治疗第19天和结束后的MRD<0.01%,接受了低强度治疗。
5年无事件生存率为89.5%(±2.2%SE),总生存率为95.5%(±1.5%SE)。5年累积复发率(CIR)为7%(95%CI,4%~11%)。
29名患者第19天检测到的MRD水平在0.001%~<0.01%之间。这些患者的5年CIR值明显高于未检出残留病灶的患者(17.2%±7.2% vs 5.3%±1.7%,P=0.02)。
综上所述,该研究表明,VLR ALL患儿采用低强度治疗可获得痊愈,表明VLR的分类标准可以通过更敏感的MRD检测来进一步完善。
原始出处:
Iman Sidhom, et al. Reduced-intensity therapy of pediatric lymphoblastic leukemia: Impact of residual disease early in remission induction. Blood. October 08, 2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#低强度化疗#
85
#ALL#
93
#MRD#
79
学习了
161
阅读谢谢分享
140
看不懂
167