PLoS One:联合生长因子抑制剂可减少糖尿病小鼠的视力损害
2012-12-28 PLoS One 互联网 prudentxiong
Figure 2. Intravitreal injection of betacellulin induces increased retinal haemorrhage and augmented retinal vascular permeability in normal and diabetic retinas. 12月17日旧金山,ClevelandClinic研究人员BelaA
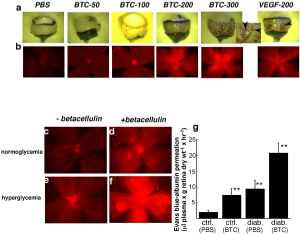
Figure 2. Intravitreal injection of betacellulin induces increased retinal haemorrhage and augmented retinal vascular permeability in normal and diabetic retinas.
12月17日旧金山,ClevelandClinic研究人员BelaAnand-Apte医生(MD和PhD)在美国细胞生物学学会年会上发言指出,一种治疗糖尿病的新方法----胰岛素和一种表皮生长因子betacellulin抑制剂联合应用----可以限制糖尿病性黄斑水肿的病变发展。
她解释说,研究采用胰岛素依赖型糖尿病小鼠,结果显示通过阻碍胰岛素和betacellulin(BTC)[betacellulin可以促进胰岛β细胞再生,胰岛β细胞再生可以贮存和释放胰岛素]之间“对话”,EGF抑制剂能够保护动物血管的完整性。
Anand-Apte医生说,“。这些试验提示,胰岛素和EGF抑制剂联合治疗可能是一种预防黄斑水肿的有效联合治疗方法,但是需要在糖尿病患者中进一步确证。”
一些在2型糖尿病、口服降糖药血糖控制不稳定、需要胰岛素治疗患者人群中进行的研究暗示了Anand-Apte医生的观点----阻碍糖尿病性视网膜病变的进展。她指出,胰岛素治疗可能会导致一些患者的视网膜病更加快速地进展,至少有一段时间存在疾病进展。她说,开始胰岛素治疗和DME发生之间存在相互关系。
另一个线索来自JudahFolkman医学博士在波士顿儿童医院的观察结果,其试验对象是接受了胰腺切除术的胰腺癌患者。因为没有胰腺产生和调节胰岛素分泌,所以这些患者会出现严重的糖尿病,但是他们很少出现增殖性视网膜病,即使当他们存活超过10到20年。研究人员大胆假设,在糖尿病患者的胰腺中,注射的胰岛素和血管通透性诱导因子分泌之间存在对话。
与凯斯西储大学和威斯康辛大学的人员合作,Anand-Apte实验室采用了糖尿病小鼠模型来观察β细胞增殖的胰腺中BTC的产生情况。在既往的研究中,Anand-Apte博士认为BTC与视网膜血管通透性增加有关。接受胰岛素治疗的糖尿病小鼠会在视网膜中产生一过性可行性betacellulin分泌高峰。在血糖过高和血糖正常小鼠的玻璃体液中注射BTC也会增加血管的通透性。
更深入地理解,研究人员确定,通过促使BTC表达,胰岛素会干扰视网膜色素细胞(RPEs)和视网膜神经周围屏障层的紧密连接。注射胰岛素首先回增加ADAM10(削弱分子细胞-细胞胶着的一种蛋白)的产生。ADAM10增加会导致BTC上调。通过短干涉RNA(siRNA)阻碍BTC和ADAM10产生,研究人员发现,他们能保护这些细胞-细胞间紧密连接。
通过使用BTC靶向EGF抑制剂,研究人员最终阻碍了BTC与胰岛素之间对话。EGF抑制剂能保留糖尿病小鼠的血管完整性。
随着时间的推移,视力损害和1型、2型糖尿病进展的关系越来越密切。国家糖尿病信息中心估计,2580万美国糖尿病患者中,420万患者具有糖尿病性视网膜病,其中675000名患者发展成最严重的形式--增殖性糖尿病视网膜病变。在增殖性糖尿病视网膜病变中,异常和渗漏的血管会侵入眼球清晰的玻璃体凝胶中,进而导致视网膜受到牵拉以及出血,最终导致视力下降。
许多伴有增殖性糖尿病视网膜病变的糖尿病患者还会出现DME----视网膜中心变厚。血-视网膜屏障中血管通透性增加会导致脂蛋白漏入视网膜中心黄斑中,导致视力急剧下降。根据美国眼科学会,DME主要的危险因素糖尿病病程延长、高血糖以及高血压。过去10年内,20%早发型(年幼发病)糖尿病和40%晚发型(年长发病)糖尿病患者会发展为DME。
与胰岛素相关的拓展阅读:
- Cell Metabolism:高胰岛素水平可导致肥胖
- 病例:二甲双胍联合胰岛素治疗的时机与获益
- 2型糖尿病患者胰岛素治疗结构化管理模式研究:一项开放、多中心、前瞻性RCT研究
- LRP16基因对胰岛素分泌和胰岛素抵抗的影响
- FDA支持新型超长效德谷胰岛素上市 更多信息请点击:有关胰岛素更多资讯

doi:10.1371/journal.pone.0013444
PMC:
PMID:
Betacellulin Induces Increased Retinal Vascular Permeability in Mice
Bela Anand-Apte, Quteba Ebrahem, Alecia Cutler, Eric Farage, Masahiko Sugimoto, Joe Hollyfield, Judah Folkman
Background Diabetic maculopathy, the leading cause of vision loss in patients with type 2 diabetes, is characterized by hyper-permeability of retinal blood vessels with subsequent formation of macular edema and hard exudates. The degree of hyperglycemia and duration of diabetes have been suggested to be good predictors of retinal complications. Intervention studies have determined that while intensive treatment of diabetes reduced the development of proliferative diabetic retinopathy it was associated with a two to three-fold increased risk of severe hypoglycemia. Thus we hypothesized the need to identify downstream glycemic targets, which induce retinal vascular permeability that could be targeted therapeutically without the additional risks associated with intensive treatment of the hyperglycemia. Betacellulin is a 32 kD member of the epidermal growth factor family with mitogenic properties for the retinal pigment epithelial cells. This led us to hypothesize a role for betacellulin in the retinal vascular complications associated with diabetes. Methods and Findings In this study, using a mouse model of diabetes, we demonstrate that diabetic mice have accentuated retinal vascular permeability with a concomitant increased expression of a cleaved soluble form of betacellulin (s-Btc) in the retina. Intravitreal injection of soluble betacellulin induced retinal vascular permeability in normoglycemic and hyperglycemic mice. Western blot analysis of retinas from patients with diabetic retinopathy showed an increase in the active soluble form of betacellulin. In addition, an increase in the levels of A disintegrin and metalloproteinase (ADAM)-10 which plays a role in the cleavage of betacellulin was seen in the retinas of diabetic mice and humans. Conclusions These results suggest that excessive amounts of betacellulin in the retina may contribute to the pathogenesis of diabetic macular edema.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#视力损害#
55
#Plos one#
54
#抑制剂#
54
#生长因子#
56