ASCO2017:BRCA突变携带者进行治疗和预防联合乳房切除术的结果分析
2017-06-06 MedSci MedSci原创
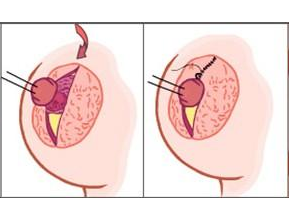
为评估遗传性乳腺癌综合征患者联合预防和/或采用立即重建和妇科风险降低手术治疗性乳房切除术的多重模式处理的效果。2012年至2016年间,对12例BRCA1和BRCA2突变的患者进行手术。手术包括双侧乳房切除术,腋窝淋巴结分期,扩张器立即重建和微创浸润性卵巢切除术并在需要时进行子宫切除术。所有手术均由专业团队在单个手术室进行。
为评估遗传性乳腺癌综合征患者联合预防和/或采用立即重建和妇科风险降低手术治疗性乳房切除术的多重模式处理的效果。2012年至2016年间,对12例BRCA1和BRCA2突变的患者进行手术。手术包括双侧乳房切除术,腋窝淋巴结分期,扩张器立即重建和微创浸润性卵巢切除术并在需要时进行子宫切除术。所有手术均由专业团队在单个手术室进行。
结果显示患者特征包括平均(+ SD)BMI为32.1±6.7(23-44)kg / m2,ASA为2.2±0.4(2-3)。58%为(7/12)绝经前妇女。患者的平均年龄为45.8±10.8(30-73)。4/12例患者进行乳腺癌治疗乳腺切除术。在4名受影响的患者中,2名患有局部晚期癌症的患者进行新辅助化疗。剩下的8/12进行预防性乳房切除术。12/12例患者进行降低风险的输卵管切除术。对75%(9/12)疑似有恶性肿瘤,平滑肌瘤,复杂子宫内膜增生,痛经和月经过多的患者,同时进行微创子宫切除术。两个妇科标本需要微型剖腹术进行去除。平均总手术时间为283.3±66.5(206-447)分钟,估计失血量(EBL)为209.2±139.2(50-500)ml。医院住院时间(LOS)为1.4±0.7(1-3)天。在比较治疗与预防性乳房切除术手术时间,EBL或LOS方面无显差异(p>
0.05)。随访显示无术后伤口感染。
研究表明,立即重建和妇科风险降低手术的联合乳房切除术术后无明显的手术并发症,而且术后无伤口感染率。虽然研究人数较少,但仍表明这种方法是可以给BRCA突变携带者的提供审慎可行的多重模式。
原始出处:
Olga
Ivanov, Nicole Centers, Karen Wiercinski, Eva Reina, et.al. BRCA mutation
carriers undergoing combined mastectomy with immediate reconstruction and
gynecologic risk-reducing surgery: An analysis of outcomes. 2017
ASCO Annual Meeting. June 3 2017.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#切除术#
59
#ASC#
60
#携带者#
65
#BRCA突变#
79
#BRCA#
76