用于区分血流感染与成人斯蒂尔病的生物标志物筛查和验证:一项前瞻性队列研究
2022-01-11 MedSci原创 MedSci原创
区分 BSI 和风湿性疾病,尤其是成人斯蒂尔病 (AOSD),仍然很困难。生物标志物筛查或许可以提供一个思路。
血流感染(BSI) 是世界范围内导致死亡的主要原因,受影响的患者数量持续增加、。BSI 疾病负担与成人的严重外伤、心肌梗塞和中风造成的负担相当 。BSI 的临床表现包括尖峰热、突然发冷、呼吸急促、心动过速、皮疹、肝脾肿大和精神变化。
BSI 可能由革兰氏阳性或阴性细菌引起。两者都含有复杂的细胞壁表面聚合物肽聚糖(PGN),它是细菌细胞壁的主要成分。磷壁酸(TA)是革兰氏阳性菌表面的多糖聚合物,按其锚定位置可分为脂磷壁酸(LTA)和壁磷壁酸(WTA)。革兰氏阴性菌也含有表面脂多糖(LPS)。PGN、LTA和LPS可以作为表面抗原,刺激外周血中的细胞,促进炎性细胞因子的释放。
AOSD 是一种罕见的、来源不明的全身性自身炎症性疾病,伴有高热、短暂性皮疹、关节痛、喉咙痛、淋巴结肿大、肝脾肿大和肌痛 。
阳性血培养仍然是 BSI 诊断的金标准。然而,血培养需要 ≥ 48-72 小时,可能会产生假阴性结果。此外,区分 BSI 和风湿性疾病,尤其是成人斯蒂尔病 (AOSD),仍然很困难。
方法
纳入标准为:(1)体温≥38℃,白细胞 ≥9.5×10 9 /L,中性粒细胞%≥75%,(2)入院时进行血培养。
排除标准为:(1)3个月内接受糖皮质激素/其他免疫抑制药物治疗的患者,(2)获得性免疫缺陷综合征/其他免疫性疾病患者,(3)入院6小时内死亡的患者。血样采集于乙二胺四乙酸 抗凝剂中入院时符合条件的患者的管子。
64 人参加了训练集(BSI 37 人,AOSD 17 人,健康对照组 10 人)。此外,86 人被纳入验证队列(BSI 67 人,AOSD 19 人)。收集临床和实验室数据。使用细菌特异性抗原刺激血样,并通过 Luminex 或酶联免疫吸附测定法检测上清液中几种细胞因子的水平。
结果
大肠杆菌和肺炎克雷伯菌是导致 BSI 最常见的病原体。在训练队列中,AOSD 患者皮疹、关节痛、肌痛、喉咙痛、淋巴结病、白细胞增多和高铁蛋白血症的发生率高于 BSI 患者。BSI 患者的降钙素原显着高于 AOSD 患者。BSI 患者的白细胞介素 (IL)-6、IL-17A、C-X3-C 基序趋化因子配体 (CX3CL)-1 和 CXC 基序趋化因子配体 10 (CXCL10) 水平高于 AOSD 患者。AOSD 患者的 IL-18 高于 BSI 患者。决策树分析表明,血浆 IL-18 和铁蛋白水平的组合可用于区分 BSI 和 AOSD(诊断准确度:97.67%,敏感性:96.15%,特异性:100%)。

训练队列中病原体的分布
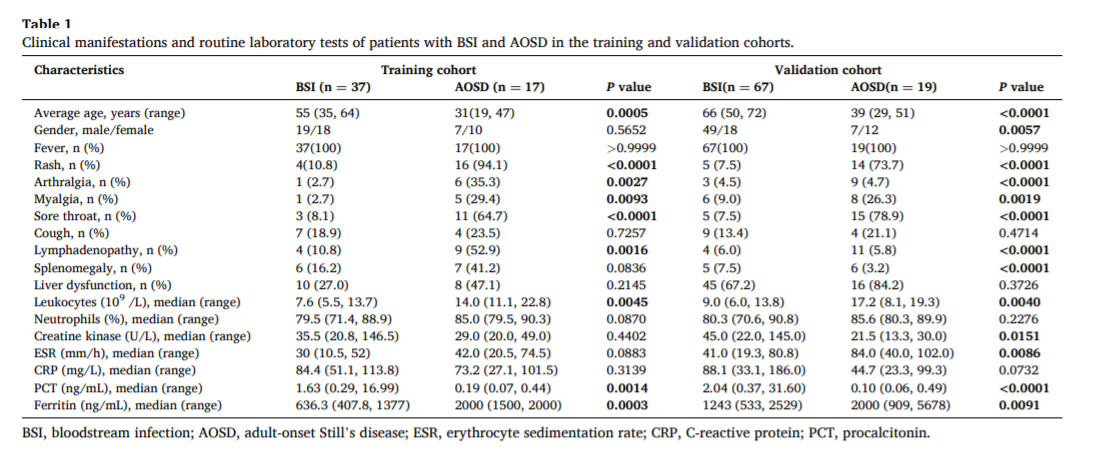
表:训练和验证队列中BSI和 AOSD患者的临床表现和常规实验室检查
结论
几种血浆细胞因子被确定为潜在的非侵入性生物标志物,以区分 BSI 和 AOSD。BSI患者血浆IL-6、IL-17A、CX3CL1和CXCL10水平高于AOSD患者,而AOSD患者血浆IL-18水平高于BSI患者。研究血浆 IL-18 和铁蛋白水平的组合可能具有更大的诊断潜力,此外,IL-18 可能是 BSI 和 AOSD 预后预测的潜在生物标志物。
来源:Wei Zhang, Tao Yang, Haocheng Zhang, Yuzhen Xu, Qingluan Yang, Qianqian Liu, Yan Gao, Jing Wu, Lingyun Shao, Wenhong Zhang,Biomarker screening and validation for the differentiation of bloodstream infection from adult-onset Still’s disease: A prospective cohort study,Cytokine,Volume 146,2021,155642,ISSN 1043-4666,
https://doi.org/10.1016/j.cyto.2021.155642.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#前瞻性#
69
#前瞻性队列#
67
#前瞻性队列研究#
81
#标志物#
51
#血流感染#
69
#生物标志#
50
#生物标志#
55