Neurology:9·11事件后退伍军人癫痫患者的多模式生活质量评估:耐药性、创伤性脑损伤和合并症的影响
2022-04-28 Naomi MedSci原创
近日,研究人员报告了不同癫痫表型生活质量对9/11事件后创伤性脑损伤(TBI)的影响。创伤后癫痫(PTE)患者的耐药性癫痫(DRE)患病率显著高于非创伤性癫痫患者,且与更高共病负担和更差生活质量相关。
癫痫是一种改变生活的疾病,由无缘无故发作的倾向定义,但癫痫的重要生理和神经精神表现不在这一定义范围内。癫痫具有不同的病因、合并症和结构灶。最近的研究表明,这些区别对于理解其对健康的影响是至关重要的,因为癫痫对身体和神经精神的影响比癫痫对预后的影响更大。例如,最近研究发现,由创伤性脑损伤(TBI)引起的癫痫,即创伤后癫痫(PTE)与以前未见报道的生活质量(QOL)有关。正如PTE可能会引起额外的QOL影响一样,其他考虑因素,如抗癫痫药物(ASM)的反应,可以以特定的方式改变身体和心理健康。例如,与非耐药癫痫患者相比,耐药癫痫患者的身体伤害和死亡率、认知障碍和精神症状发生率更高。然而,关于DRE、PTE和其他生理/神经精神疾病如何相互作用和调节生活质量,人们知之甚少。
对影响PTE生活质量的因素有更深入的了解,这对于促进努力确定生活质量差的风险最大的个人,以及确定有效的干预措施以减轻/预防不良的健康状况和/或生活质量至关重要。例如,与非耐药癫痫(DRE)患者相比,耐药癫痫(DRE)患者的身体损伤和死亡率、认知障碍以及精神症状的发生率更高。然而,关于DRE、PTE和其他生理/神经精神疾病如何相互作用和调节生活质量,人们知之甚少。对影响PTE生活质量的因素有更深入的了解,这对于促进努力确定生活质量差的风险最大的个人,以及确定有效的干预措施以减轻/预防不良的健康状况和/或生活质量至关重要。
生活质量是一个复杂的概念,它涉及到一个人在其价值体系和文化背景下对其生活的评估,并受到个人标准、期望、目标和担忧的影响。对生活质量的评估可以是一般性的,也可以是具体的。例如,癫痫特定的测量被用来量化药物、癫痫发作担忧、情绪和癫痫患者(PWE)功能状态的影响,但这些测量可能不能解决更广泛的复杂的生活质量。近日,有研究人员报告了不同癫痫表型的生活质量对9/11事件后高发生率创伤性脑损伤(TBI)退伍军人的影响。
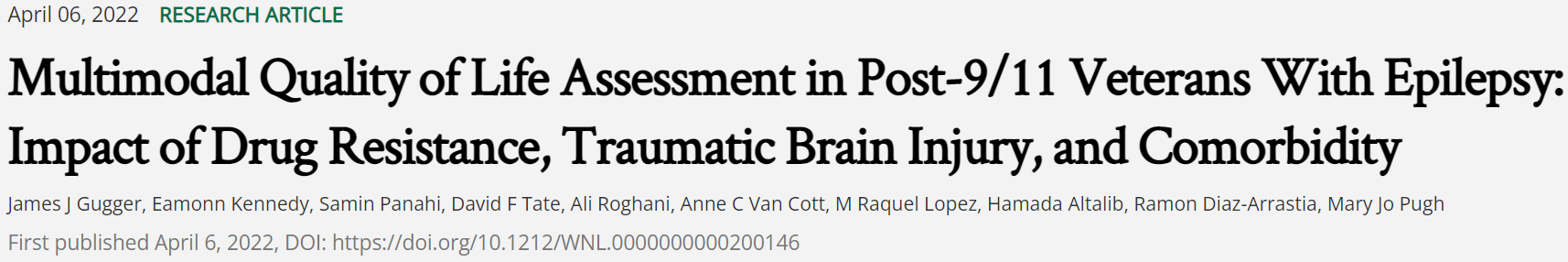
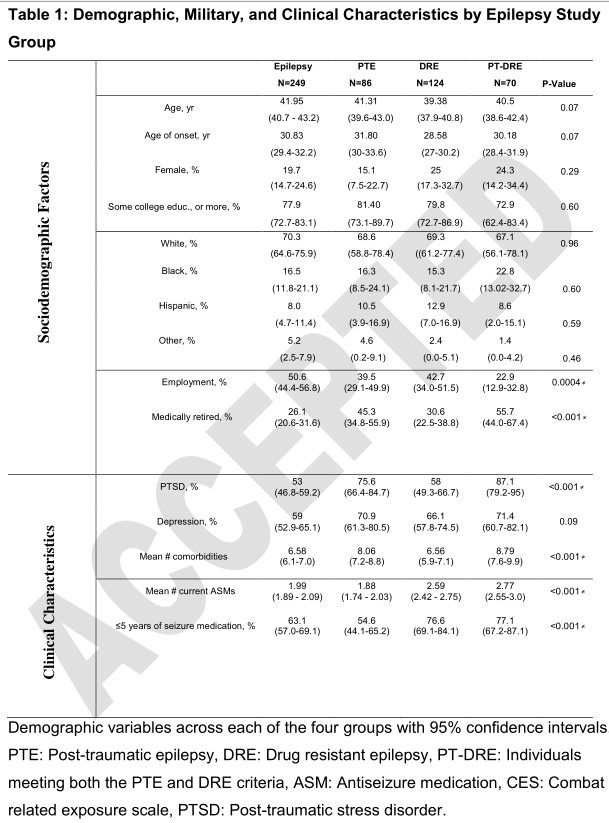
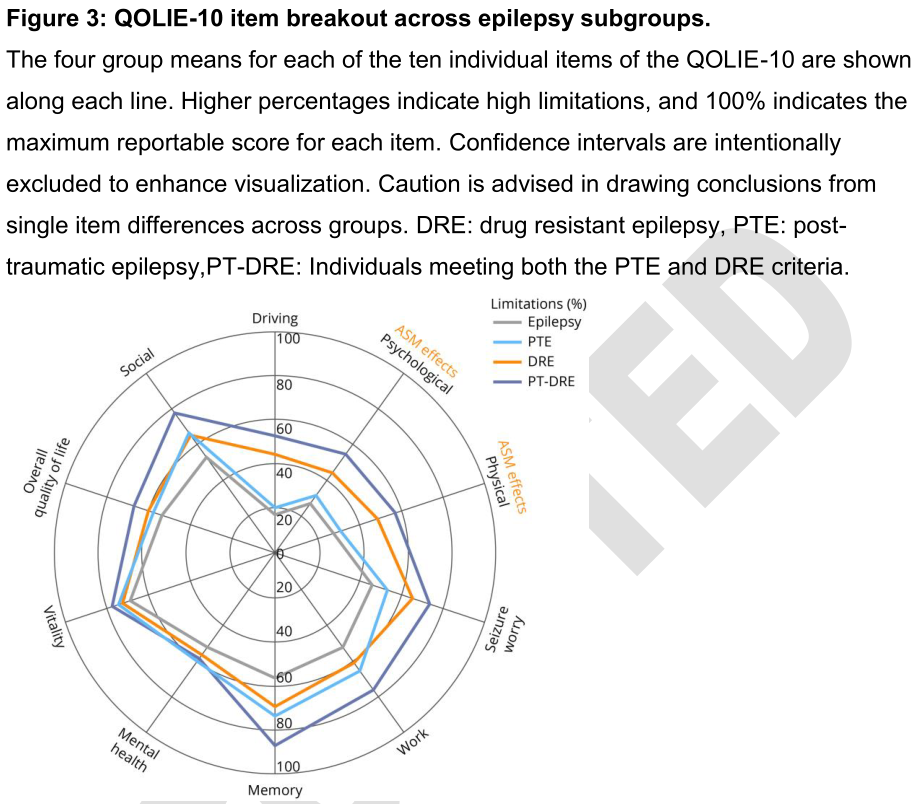
这项来自退伍军人健康管理局的观察性队列研究包括9/11事件后患有癫痫的退伍军人。采用癫痫识别算法、图表提取和自我报告措施相结合的方法将患者分为四组:1.药物控制的癫痫;2.耐药癫痫(DRE);3.创伤后癫痫(PTE);或4.耐药创伤后癫痫(PT-DRE)。根据年龄、性别和合并症的数量进行调整,比较了不同组别的六项生活质量指标的总分。
- 共有529名癫痫患者进入分析:249名对照组(即无DRE或PTE的癫痫患者)、124名DRE患者、86名PTE患者和70名PT-DRE患者。
- 与非创伤性癫痫相比,耐药性癫痫在PTE患者中更为常见(45%比33%,优势比1.6(95%CI:[1.1-2.4],p=0.01))。
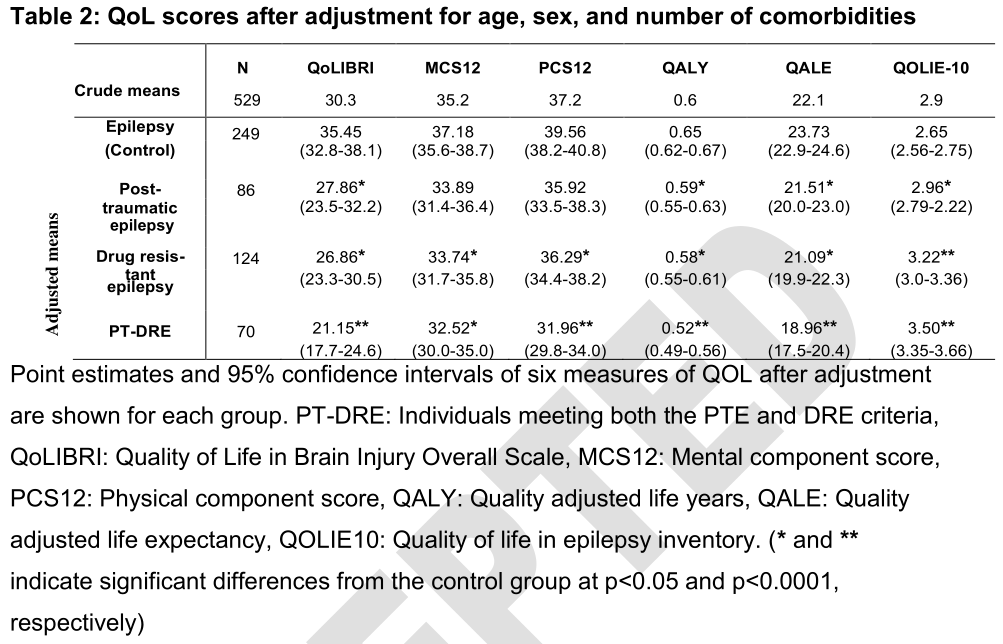
- 在健康记录中,PTE和PT-DRE患者比那些非创伤性癫痫患者有更多的共病情况。同时患有PTE和DRE的患者报告的生活质量在所有六项指标中都是最低的,在对共病情况进行调整和进一步的线性分析后,这种情况仍然存在。
在PTE患者中,DRE患病率显著高于非创伤性癫痫患者。与非创伤性癫痫患者相比,PTE还与更高的共病负担和更差的总体生活质量有关。PTE患者明显容易受到与脑外伤和癫痫相关的共病的影响。这一高危人群应该成为未来研究的重点,旨在阐明与不良健康结果相关的因素,并开发抗癫痫疗法。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言





















#退伍军人#
114
#癫痫患者#
75
#Neurol#
96
#合并症#
110
#创伤性#
91
#期刊论坛#哦
74
#创伤#
91
#损伤#
100