European Radiology:放射学列线图在cHCC-CC和ICC术前鉴别中的应用
2022-04-16 shaosai MedSci原创
混合型肝细胞-胆管癌(cHCC-CC)十分少见,但由于其独特的生物学、组织病理学和临床特征,在临床和病理学上越来越受到关注。
 现阶段,临床上普遍认为混合型肝细胞-胆管癌(cHCC-CC)来自于同时表达胆管和肝细胞的肝母细胞,占原发性肝脏恶性肿瘤的0.4-14.2%。而肝内胆管细胞癌(ICC)是仅次于肝细胞癌(HCC)的第二大原发性肝脏恶性肿瘤,起源于肝内胆管上皮。
现阶段,临床上普遍认为混合型肝细胞-胆管癌(cHCC-CC)来自于同时表达胆管和肝细胞的肝母细胞,占原发性肝脏恶性肿瘤的0.4-14.2%。而肝内胆管细胞癌(ICC)是仅次于肝细胞癌(HCC)的第二大原发性肝脏恶性肿瘤,起源于肝内胆管上皮。
尽管cHCC-CC十分少见,但由于其独特的生物学、组织病理学和临床特征,在临床和病理学上越来越受到关注。对于大多数可切除的原发性肝脏恶性肿瘤患者来说,手术仍然是主要的治疗手段。具报道,cHCC-CC切除后的生存率低于HCC,与ICC相似。因此,在手术前对cHCC-CC进准确诊断意义重大,对进一步的治疗指导起到关键作用。
在目前的临床实践中,计算机断层扫描(CT)和磁共振成像(MRI)已被广泛用于肝脏肿瘤的检测和定性。然而,由于这两种肿瘤的复杂影像特征和罕见性,通过影像学研究对cHCC-CC进行术前诊断仍然非常困难。cHCC-CC的影像学特征不仅包括HCC的典型特征,还包括ICC的特征。据报道,几乎有三分之二的cHCC-CC患者出现影像学误诊。肝脏特异性MR对比剂,如钆塞酸,既可作为细胞外对比剂使用,同时又被肝细胞特异性摄取,因此越来越多地被用于肝脏病灶的评估。
放射组学通过从放射图像中提取大量的定量特征,可以提供整个潜在的肿瘤内异质性和癌症表型的重要信息。以前的研究表明,放射组学在描述病变特征、评估肿瘤和评价患者对肝脏治疗的反应方面具有良好的能力。
近日,发表在European Radiology杂志的一项研究开发了一个基于动态对比增强(DCE)MR图像的用于术前区分cHCC-CC和IMCC的放射组学列线图,为临床术前制定最佳治疗方案并预测患者预后提供了强有力的技术支持。
本项研究共纳入了151名训练队列患者(45名cHCC-CC和106名IMCC)和65名验证队列患者(19名cHCC-CC和46名IMCC)。对临床特征和MR特征的结果进行了分析,并从DCE-MR图像中提取了放射组学特征。通过最小绝对收缩率和选择算子算法,根据放射组学特征建立了放射组学特征。采用单变量和多变量分析来确定重要的临床放射学变量并构建临床模型。然后通过多变量逻辑回归分析,将放射组学特征和重要的临床放射学变量纳入放射组学列线图。通过受试者工作特征曲线评估放射组学列线图、放射组学特征和临床模型的性能,并比较了曲线下面积(AUC)。
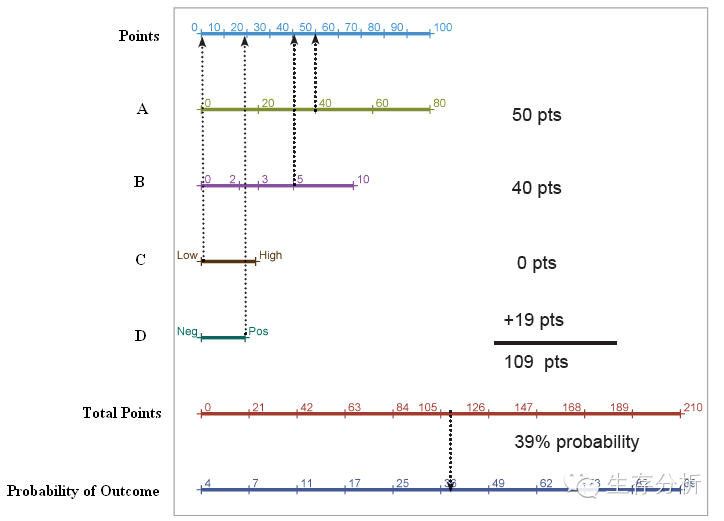
本研究共选择了11个放射组学特征来开发放射组学特征。整合了甲胎蛋白、背景肝病(肝硬化或慢性肝炎)和放射组学特征的放射组学列线图显示出了良好的校准和鉴别性能,训练队列的AUC值为0.945,验证队列为0.897。放射组学特征和临床模型的AUC在训练队列中分别为0.848和0.856,在验证队列中为0.792和0.809。放射组学列线图的表现优于单独使用放射组学或临床模型(P < 0.05)。
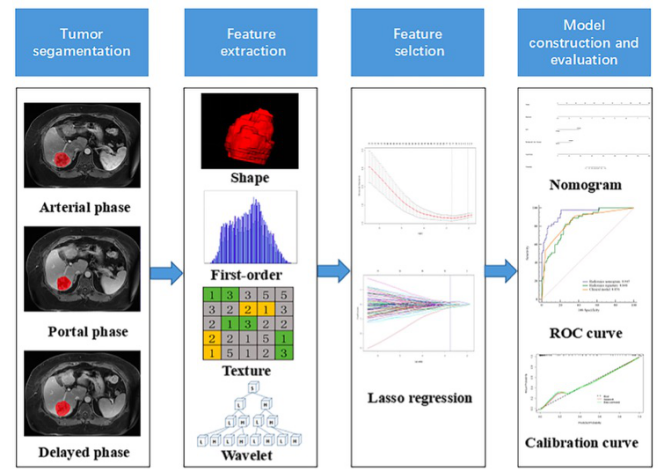
图 在本研究中进行DCE-MR的放射组学分析的关键步骤的工作流程
综上所述,本研究提出了一个包含放射组学特征和临床因素的放射组学列线图,可以作为术前区分cHCC-CC和IMCC的无创影像学工具。
原文出处:
Yang Zhou,Guofeng Zhou,Jiulou Zhang,et al.DCE-MRI based radiomics nomogram for preoperatively differentiating combined hepatocellular-cholangiocarcinoma from mass-forming intrahepatic cholangiocarcinoma.DOI:10.1007/s00330-022-08548-2
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#列线图#
68
#PE#
52
#HCC#
62
#放射学#
62
#ICC#
61
#CHC#
64