Nat Commun:多发性硬化症——通过帮助细胞来帮助自己
2019-01-30 佚名 生物通
多发性硬化等疾病的特征是“髓鞘”受损,髓鞘是一种包裹在神经细胞周围的保护层,类似于电线周围的绝缘层。柏林夏利特大学的研究人员发现了人体如何启动修复机制,保护髓鞘减少损伤。他们的研究结果为开发治疗多发性硬化症的新药奠定了基础,并发表在Nature Communications杂志上。
多发性硬化等疾病的特征是“髓鞘”受损,髓鞘是一种包裹在神经细胞周围的保护层,类似于电线周围的绝缘层。柏林夏利特大学的研究人员发现了人体如何启动修复机制,保护髓鞘减少损伤。他们的研究结果为开发治疗多发性硬化症的新药奠定了基础,并发表在Nature Communications杂志上。
多发性硬化症是中枢神经系统最常见的自身免疫性疾病。据估计,仅在德国就有20多万人受到这种疾病的影响。患有多发性硬化症的人会出现视力和感觉问题,以及协调能力受损甚至瘫痪。这些症状是由大脑或脊髓神经冲动的破坏引起的。当身体的免疫系统攻击髓鞘时,就会发生这种破坏,髓鞘包裹着身体的神经纤维,并提供电绝缘。当髓鞘不再完整时,神经细胞之间的通讯就会受到损害。全世界的研究人员都在寻找修复髓鞘的新方法,同时也在寻找减轻多发性硬化症患者神经症状的方法。来自柏林夏利特大学的研究人员已经朝着这个目标迈出了决定性的一步。
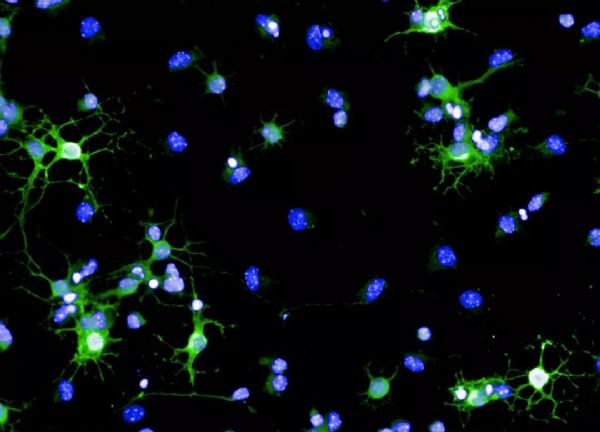
柏林夏利特大学的研究小组决定更仔细地观察身体自我修复的先天能力,知道在某些条件下,中枢神经系统能够修复髓鞘的损伤。特定的分子信号使干细胞分化成髓鞘修复细胞(少突胶质细胞),这些细胞位于大脑中的一个小的干细胞巢中。一旦它们离开这个位置,这些修复细胞就会迁移到发生髓鞘损伤的地方,以恢复受影响的神经细胞的电绝缘性。到目前为止,对引起这种髓鞘再生机制的分子信号知之甚少。“我们发现,Chi3l3蛋白在机体产生新的能形成髓鞘的少突胶质细胞的能力中起着核心作用。”该文章的第一作者,柏林夏利特大学的医学免疫学研究所Sarah-Christin Staro?om博士说。作为神经治疗卓越集群和实验与临床研究中心(ECRC)的研究员,Staro?om博士对该蛋白做了如下的解释:“Chi3l3蛋白启动神经干细胞向髓鞘修复细胞分化,修复受损神经细胞周围的电绝缘性。”
利用小鼠模型,研究小组能够证明大脑中的Chi3l3蛋白水平的降低显著损害了身体产生少突胶质细胞的能力,而Chi3l3蛋白的输注可以使髓鞘修复细胞的产生增加。使用人类细胞进行体外实验时,同样的反应被观察到。“我们希望利用这一知识开发出新一代药物,用于治疗多发性硬化症。”Staro?om博士解释说,“作为下一步,我们将更详细地研究是否可以使用Chi3l3或相关蛋白来减轻多发性硬化患者的神经症状。”
原始出处:Sarah C. Starossom, Juliana Campo Garcia, Tim Woelfle, et al. Chi3l3 induces oligodendrogenesis in an experimental model of autoimmune neuroinflammation. Nat Commun. 15 January 2019
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#COMMUN#
89
#硬化症#
100
#Nat#
76
#多发性#
99