Mov Disord: 帕金森:脑脊液中的哪些蛋白,影响突触核蛋白的稳态
2021-08-08 Freeman MedSci原创
与神经递质分泌、突触可塑性和内溶酶体自噬有关的CSF蛋白,可能作为PD和DLB中与α-突触核苷酸蛋白稳态有关的生物标志物。
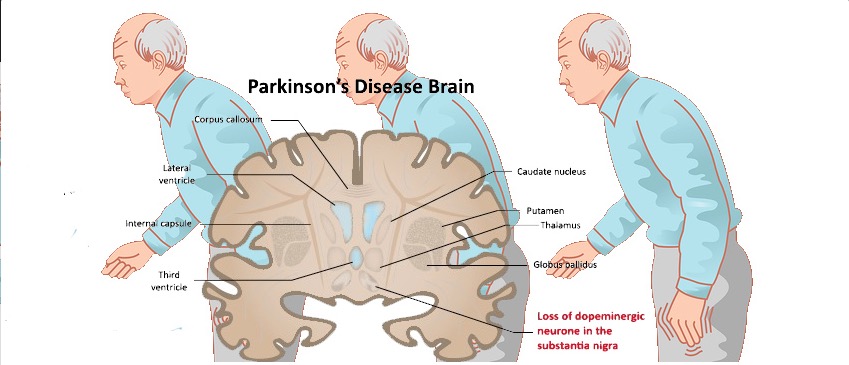
在大多数α-突触核蛋白病患者中,如帕金森病(PD)和路易体痴呆(DLB),其共同的病理特征是α-突触核蛋白的异常构象的聚集。
随后,在遗传研究以及细胞和动物模型中发现了几个与α-synuclein蛋白稳态有关的分子途径。这些途径包括自噬功能受损,例如内溶酶体功能障碍、泛素-蛋白酶体系统、线粒体稳态和突触可塑性。
尽管有这些明确的证据表明涉及的途径,但缺乏有效的生物标志物,这些标志物在人类生物流体中是明确的疾病和/或途径特异性的。
最近的一项研究,使用固相萃取法结合平行反应监测质谱法(solid-phase extraction combined with parallel reaction monitoring mass spectrometry ),对3组帕金森病患者、阿尔茨海默病(AD)患者和健康对照组的脑脊液(CSF)中与自噬性内溶酶体和泛素蛋白酶体功能相关的肽/蛋白质谱进行了有针对性的探索。
有趣的是,PD患者的溶酶体相关膜糖蛋白1和2(LAMP1和LAMP2)、 cathepsin F (CTSF)、神经节苷脂GM2激活剂(GM2A)、AP-2复合体亚单位β(AP2B1)和泛素的CSF蛋白水平低于AD患者、前驱AD患者和健康对照者。
随着技术的进步,最近的一个无偏见的定量蛋白质组学(unbiased quantitative proteomics approach )方法,使用液相色谱-串联质谱,报告了与神经递质分泌有关的蛋白质(颗粒蛋白家族)的CSF水平下降,以及与健康对照组相比,散发性PD患者的粘连结(adherens junctions )。
具体来说,PD患者的神经分泌蛋白VGF、secretogranin 2(SCG2)、secretogranin和secretogranin、chromogranin-A(CHGA)和chromogranin-B以及cadherins的CSF蛋白水平都较低。
根据这一证据,德国图宾根大学的Stefanie Lerche等人,探究了与α-synuclein蛋白稳态途径相关的CSF蛋白谱,在2个大型单中心的α-synuclein病症队列中(共385名PD患者和67名DLB患者),并将其与健康对照组相比。
由于溶酶体伴侣介导的自噬功能受损,代表了PD的一个关键机制,他们特别纳入了葡萄糖苷酸酶(GBA)基因有变异的PD患者(385人中的80人)和DLB患者(67人中的17人)。
鉴于DLB患者与PD相比,以及GBA变体患者与野生型患者相比,α-突触蛋白的病理变化加快,临床轨迹明显,主要假设是,这些患者群体的情况将更加不同。
他们发现:
(1)与健康对照组相比,PD和DLB患者中与神经递质分泌、突触可塑性和内溶酶体自噬有关的蛋白质含量较低。
(2) 这些模式在DLB患者中比在PD患者中更明显,在这两个实体中,GBA变体状态更突出。
(3) 这些蛋白的CSF水平与总α-突触核蛋白的CSF水平呈正相关,即:蛋白稳态低的那些蛋白,含量更低,且与总α-突触核蛋白的低水平有关。
(4) 这些发现可被纵向证实。与蛋白酶谱正常的PD患者相比,CSF蛋白酶谱低的PD患者,在纵向上,显示出较低的α-synuclein水平。
这个研究的重要意义在于发现了:与神经递质分泌、突触可塑性和内溶酶体自噬有关的CSF蛋白,可能作为PD和DLB中与α-突触核苷酸蛋白稳态有关的生物标志物。
原文出处:
Lerche S, Sjödin S, Brinkmalm A, et al. CSF Protein Level of Neurotransmitter Secretion, Synaptic Plasticity, and Autophagy in PD and DLB. Mov Disord. Published online June 28, 2021:mds.28704. doi:10.1002/mds.28704
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















#稳态#
117
#核蛋白#
112
#Dis#
94
#突触#
96
#Disord#
101
有意思
103