J Clin Oncol:ROCK2抑制剂贝鲁地尔可有效治疗难治性慢性移植物抗宿主病
2021-04-23 MedSci原创 MedSci原创
贝鲁地尔治疗可使患者获得高ORR和总存活率,且同时可改善患者的生活质量、减少CS剂量和限制性毒性
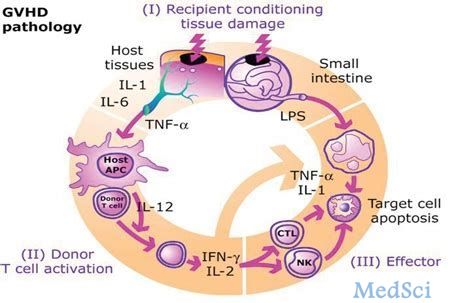
与rho相关的卷曲螺旋蛋白激酶2(ROCK2)信号传导通路调节Th17/调节性T细胞平衡并控制纤维化途径。用贝鲁地尔(belumosudil,KD025)选择性抑制ROCK2可能为治疗慢性移植物抗宿主病(cGVHD)提供一种新方法。

近日发表在“Journal of Clinical Oncology”上的一项IIa期、开放标签的剂量探索性研究“ROCK2 Inhibition With Belumosudil (KD025) for the Treatment of Chronic Graft-Versus-Host Disease”,旨在明确贝鲁地尔用于既往接受过一线-三线治疗(LOT)的cGVHD患者中的剂量和效果。主要终点是总体缓解率(ORR)。
共招募了54位cGVHD患者,从确诊cGVHD到招募入组的中位时间为20个月。78%的患者为重度cGVHD,50%的患者至少累及4个器官,73%的为末次LOT难治性cGVHD,50%的患者既往至少接受了三线治疗。
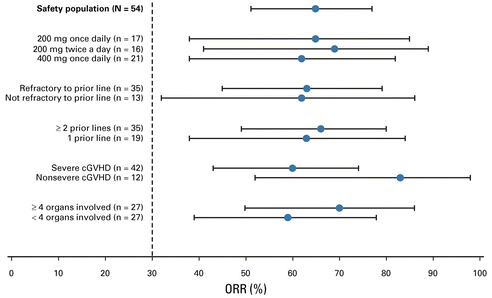
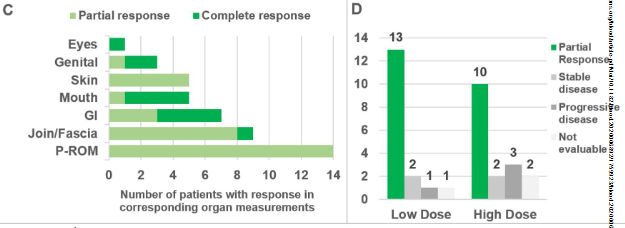
不同分组的缓解率
中位随访29个月,贝鲁地尔用药剂量为200 mg·1/日、200 mg·2/日和400 mg·1/日时的ORR(95% CI)分别为65% (38%-86%)、69% (41%-89%)和62% (38%-82%)。
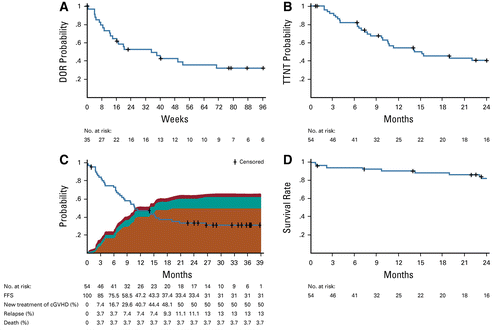
贝鲁地尔治疗缓解持续时间
缓解率具有临床意义,中位缓解持续时间为35周,且与生活质量提高和皮质类固醇(CS)用量减少相关。19%的患者停用CS治疗。
6个月和12个月时的无失败存活率分别为76%(62%-85%)和47%(33%-60%)。2年总存活率为82%(69%-90%)。
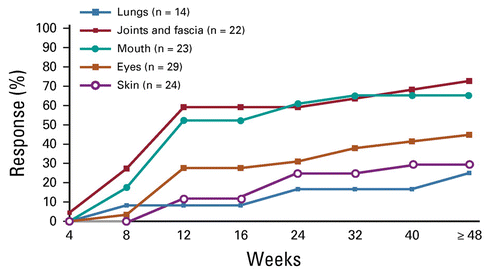
不同器官的缓解率
贝鲁地尔的耐受性良好,血细胞减少症的发生率低。未发生预期之外的不良反应,感染风险(包括巨细胞病毒感染和再激活)未见明显增加。
总之,贝鲁地尔治疗可使患者获得高ORR和总存活率,且同时可改善患者的生活质量、减少CS剂量和限制性毒性。该研究结果提示贝鲁地尔或可成为难治性cGVHD患者的有效选择。
原始出处:
Madan Jagasia, et al. ROCK2 Inhibition With Belumosudil (KD025) for the Treatment of Chronic Graft-Versus-Host Disease. J Clin Oncol. https://creativecommons.org/licenses/by-nc-nd/4.0/
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#植物#
62
#Oncol#
53
#ROC#
76
#ROCK#
65
#抑制剂#
65
#2抑制剂#
55
#J Clin Oncol#点击查看更多该期刊内容
120
#宿主#
74
#移植物抗宿主病#
75
#难治性#
42