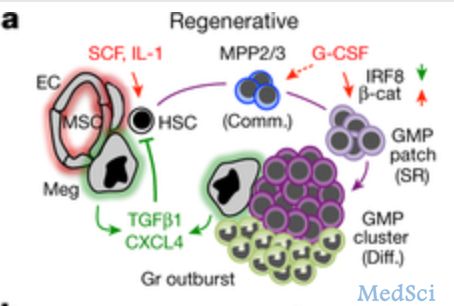
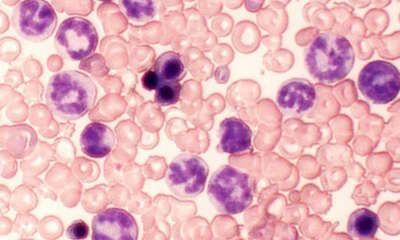
Nature:造血细胞在骨髓内的动态调控
2017-03-31 Leo.C MedSci原创
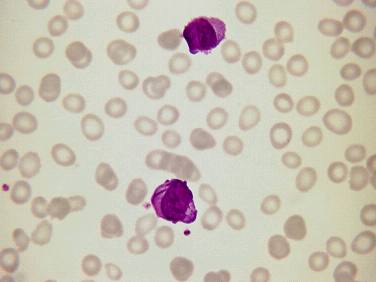
骨髓内血细胞的形成,然后一步步分化为颗粒性细胞和巨噬细胞的原始细胞,再才逐步分化为颗粒性细胞和巨噬细胞,这一过程可以通过单细胞RNA测序技术来追踪和鉴别这一过程所产生的基因调整及变化。但是我们对于这一变化在骨髓中发生的空间结构的变化了解甚少。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#血细胞#
82
#Nat#
78
非常好的研究
101
不错的指南,为我们探讨研究提供了方针,给点个赞了!
127
#造血#
70
#造血细胞#
74