Alz Res Therapy:阿尔兹海默和路易体痴呆,APOE ε4对认知表现的影响不同
2021-11-05 Freeman MedSci原创
与非携带者相比,APOE ε4携带者的特定初始认知症状的几率在ADP和LRP之间存在差异。
众所周知,阿尔茨海默病(AD)在其典型的临床表现中,早期表现为发作性记忆障碍,随着疾病的发展,其他认知领域包括视觉空间、语言和执行功能也逐渐出现障碍。注意到的基本病理变化是神经元淀粉样β斑块和神经纤维缠结的负担越来越重。人们已经认识到早期临床症状与常见的健忘症表现有很大的异质性,国际工作组(IWG)-2临床诊断标准中正式规定了非典型的非健忘症表型。生物标志物的差异,包括CSF总tau和MRI成像,在那些有早期健忘症和非健忘症症状(主要是语言、执行或视觉空间功能障碍的初始症状)以及神经纤维缠结的模式,表明可能有潜在的生物特征影响初始主要临床症状的早期表现。
年龄和遗传状况似乎在AD的早期临床表型中起作用。AD的早期非雄性表现在年轻发病的AD中报道得更多。载脂蛋白ε4(APOE ε4)等位基因最常与晚期AD的风险增加有关,与健忘的表现有关。
APOE ε4等位基因在失忆型AD中的流行率增加也提出了这样的假设:APOE ε4是一个解剖学上的选择性风险因素,它增加了记忆相关的内侧颞区对AD病理的脆弱性(ADP),它可能通过影响特定的大规模脑网络来调节AD的临床表型。也有报道说,APOE ε4携带者的比例在AD的失语变体中没有升高。
这些发现在AD中提出了进一步的问题:一是APOE ε4等位基因是否对AD的其他非失语临床症状(执行、视觉空间)有不同的影响;二是APOE ε4携带者与阿尔茨海默病的基础神经病理学不同,是否也对失语症状有类似的易感性。
路易体痴呆(DLB)是最常见的痴呆形式之一,其特点是与路易相关的病理学(LRP),包括α-突触蛋白免疫阳性的神经元内含物(路易体)和过程(路易性神经纤维)。许多患有LRP的受试者还显示出同时存在的ADP(ADP-LRP)。APOE ε4等位基因是整个路易体疾病谱的一个强有力的风险因素,甚至在没有并存ADP的纯突触蛋白病的情况下也会增加出现痴呆的可能性。与AD相比,路易体痴呆患者的注意力、视觉空间和视觉结构障碍往往是主要的认知领域差异,但他们往往也有不同的记忆障碍。
有人提出了一个与帕金森病的神经病理学和认知有关的路易体痴呆的渐进式分期系统,DLB患者被认为显示了这种相同的皮质受累顺序。在这种情况下,APOE ε4携带者状态如何影响失忆或其他非失忆认知领域的几率,包括LRP患者和ADP-LRP混合病理的患者的视觉空间障碍,尚不清楚。
因此,克利夫兰诊所的 Jagan A. Pillai等人, 在国家阿尔茨海默氏症协调中心(NACC)的数据集中进行了目前的研究,该数据集包括美国多个地点的高度确定的队列,大部分参与者都有神经病理学信息,对此进行探究。
他们对国家阿尔茨海默氏症协调中心数据库中2288名神经病理学证实为ADP或LRP的参与者进行了回顾性队列研究,他们有初始认知症状记录,并且临床痴呆评级-全球(CDR-G)得分≤1(认知正常,MCI或早期痴呆)。考虑到评估时的年龄、性别和教育程度的未经调整和调整的逻辑回归模型检查了APOE ε4基因型与有LRP的ADP组和ADP-LRP组初始症状(记忆、执行、语言视觉空间)之间的关系。
共133名参与者符合单独的ADP标准,90名符合单独的LRP标准,895名符合ADP和LRP(ADP-LRP)并存的标准。在所有三组中,年龄较小的人出现非家庭症状的几率增加。在ADP的调整模型中,APOE ε4携带者比非携带者有更高的失忆初始症状几率1.5 [95% CI, 1.7-2.14, p = 0.003]和更低的初始语言症状几率0.67 [95% CI, 0.47-0.96, p = 0.03] 。
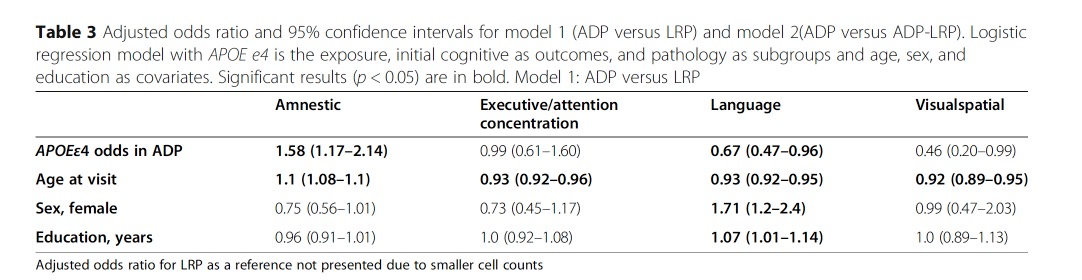
这两种症状的几率在ADP和ADP-LRP混合组之间没有区别。在调整后的模型中,女性性别和高等教育增加了ADP组初始语言症状的几率。在未经调整的模型中,APOE ε4携带者与LRP的视觉空间初始症状的几率较高,为21.96 [95% CI, 4.02-110.62, p < 0.0001],而初始执行/注意力症状没有差异。
在LRP中,APOE ε4对失忆症状的几率并不显著;然而,评估ADP和LRP组之间失忆症状的几率差异的交互作用也没有达到统计学意义。
这个研究的重要意义在于发现了:与非携带者相比,APOE ε4携带者的特定初始认知症状的几率在ADP和LRP之间存在差异。ADP APOE ε4携带者出现初始遗忘症状的几率更高,LRP APOE ε4携带者出现视觉空间初始症状的几率更高。这支持了APOE ε4与潜在的神经病理学一起对初始认知症状产生不同影响的假说。
原文出处:
Pillai JA, Bena J, Bonner-Jackson A, Leverenz JB. Impact of APOE ε4 genotype on initial cognitive symptoms differs for Alzheimer’s and Lewy body neuropathology. Alz Res Therapy. 2021;13(1):31. doi:10.1186/s13195-021-00771-1
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言




















#ERA#
79
#认知表现#
70
#路易体#
86
#阿尔兹海默#
99
#APOE#
83
老年性痴呆,未来还是希望借助神经电生理吧,也许更为有效!
78