下尺桡关节脱位(distal radioulnar joint dislocation)
2022-03-21 Dr. zhang 骨科青年
下尺桡关节的主要功能是维持前臂旋转时的稳定,其损伤与脱位未得到良好治疗会导致慢性腕部疼痛、前臂旋转功能受限、骨关节炎等严重后果。
下尺桡关节的主要功能是维持前臂旋转时的稳定,其损伤与脱位未得到良好治疗会导致慢性腕部疼痛、前臂旋转功能受限、骨关节炎等严重后果。
01下尺桡关节的功能与解剖
-
尺侧副韧带:附着于尺骨茎突尖与三角骨、豌豆骨
-
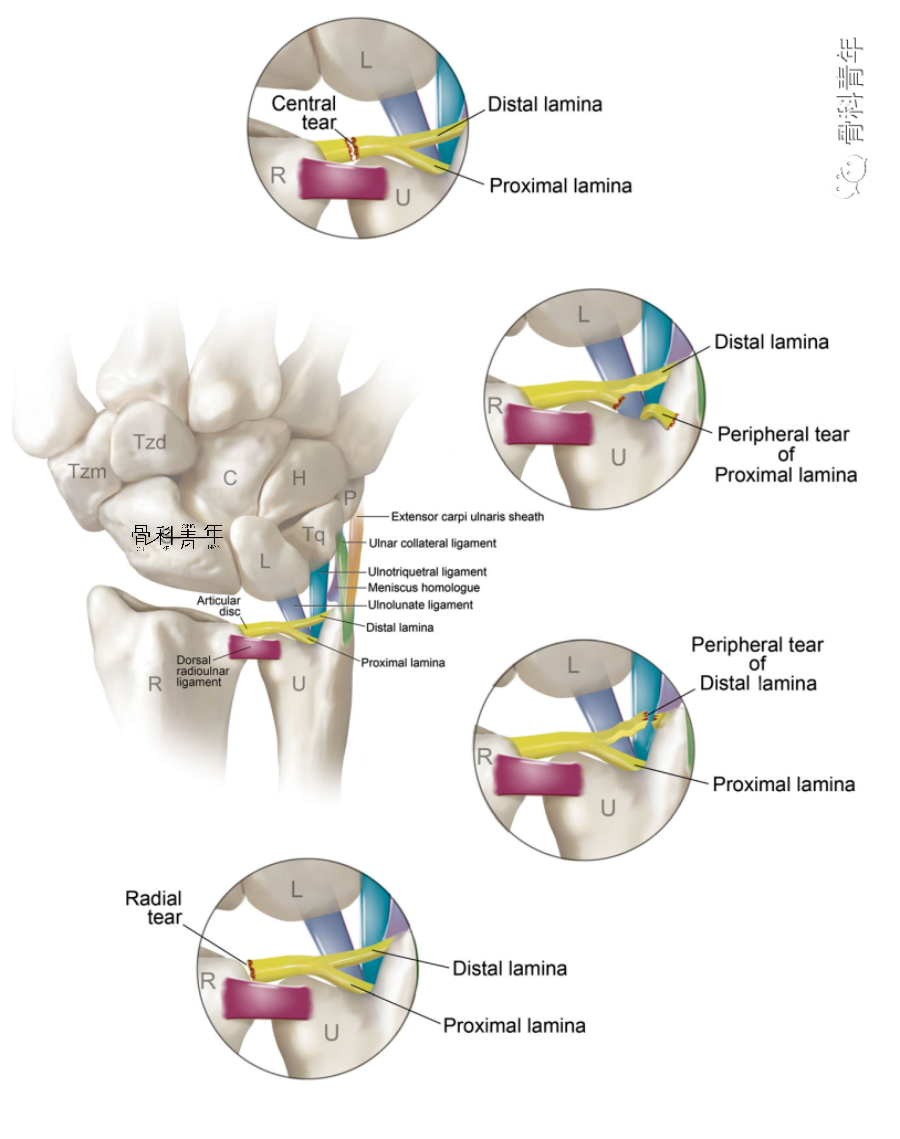
关节软骨盘(TFCC):附着于尺骨茎突基底与桡骨已状切迹边缘
-
桡尺掌侧韧带/桡尺背侧韧带:为关节囊的一部分
-
旋前方肌:连接尺桡骨远端,起自尺骨,止于桡骨

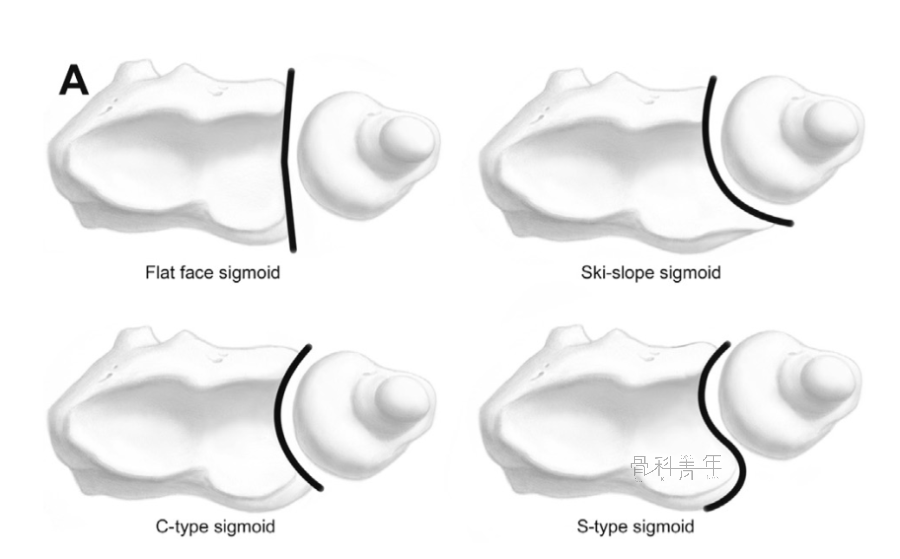
乙状切迹的解剖变异与下尺桡关节稳定性也存在相关性。平坦或者较浅的乙状切迹沟使下尺桡关节脱位概率增加,而较深的乙状切迹沟则相反。
图示乙状切迹的解剖变异(平坦型、滑雪板型、C型、S型):
02 损伤机制
-
掌侧脱位:下尺桡掌侧韧带断裂时,旋后过程会发生尺骨小头向掌侧的半脱位。掌侧脱位由于旋前方肌的牵拉,导致尺桡骨发生重叠
掌侧脱位
-
背侧脱位:下尺桡背侧韧带断裂时,旋前过程即会发生尺骨小头向背侧的半脱位。背侧脱位由于旋前方肌的阻挡,尺桡骨不会发生明显重叠
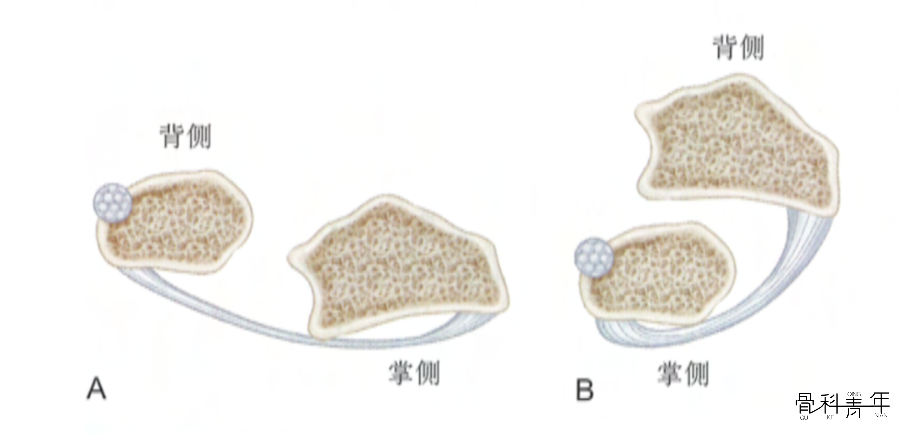
完全的尺骨头脱位伴有尺骨茎突基底部的骨折或TFCC的完全断裂,上述结构完整的情况下不会发生尺骨头脱位。
03临床表现与诊断
下尺桡关节脱位具有如下表现:
-
腕关节疼痛: 局限于下尺桡关节及尺骨茎突处,腕关节旋转及尺偏时疼痛加重; -
局部肿胀:一般较轻; -
局部弹性隆起:尺骨头向背侧或掌侧隆起,压之复位,抬手即弹回原处;即“琴键”征; -
活动受限:因疼痛患侧前臂旋转及尺偏明显受限,伴有三角软骨损伤时尤甚。
04 治疗
-
背侧脱位患者,予以旋后位短臂石膏固定4-6周;
-
掌侧脱位患者,予以旋前位短臂石膏固定4-6周。
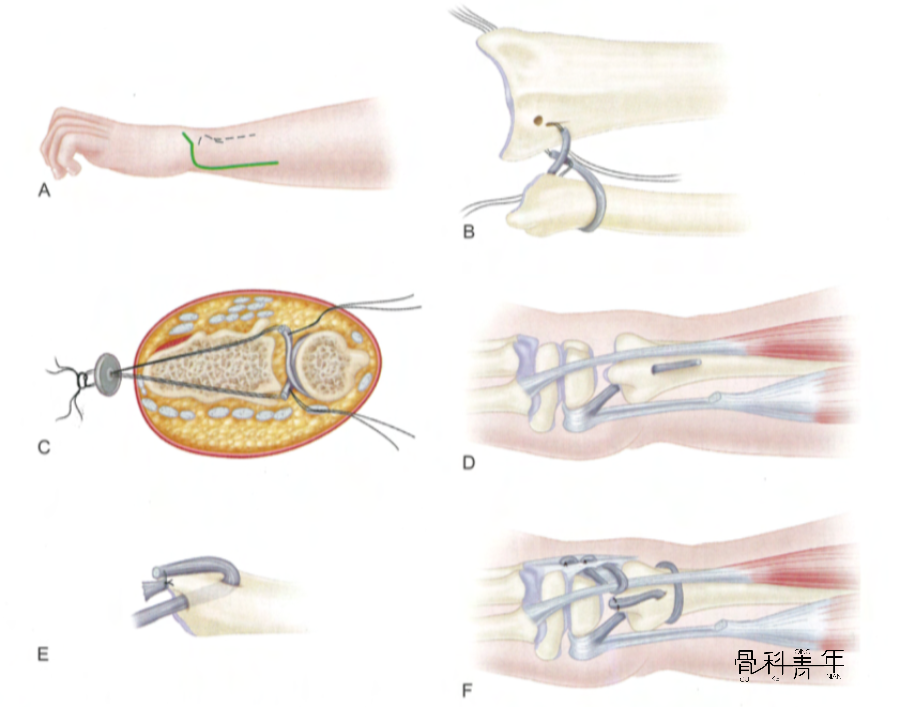
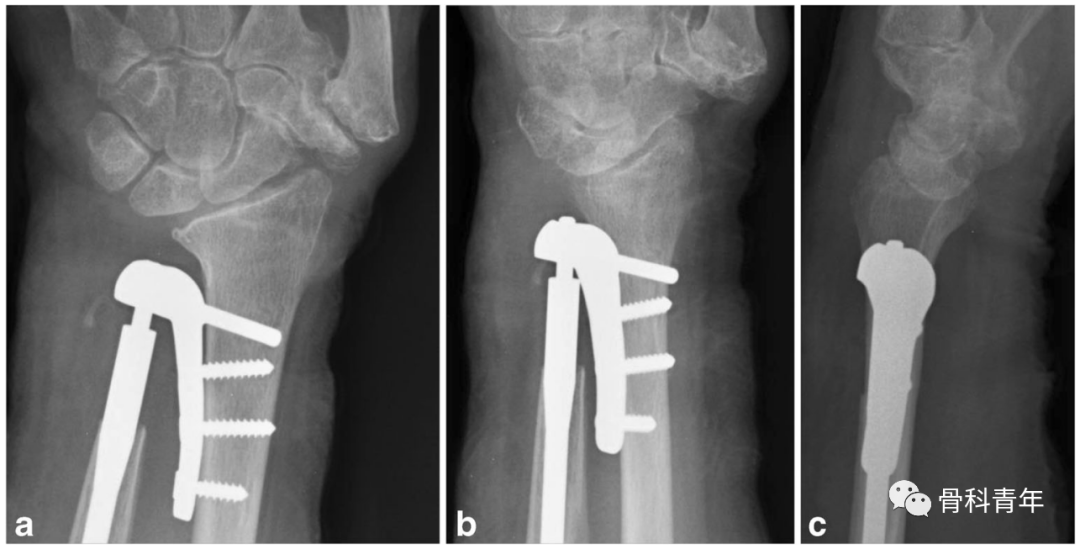
对急性下尺桡关节脱位,可行克氏针固定尺桡骨:

① Sauvé-Kapandji法及其改良
该方法于1997年提出,通过在尺骨小头近端截骨,骨性融合下尺桡关节,但该方法存在尺骨残端不稳等并发症,其后出现各种改良方法,包括旋前方肌填塞骨间隙、尺侧腕伸肌韧带加强等方法。

② 稳定下尺桡关节韧带的Bunnell方法(来源:坎贝尔骨科手术学)
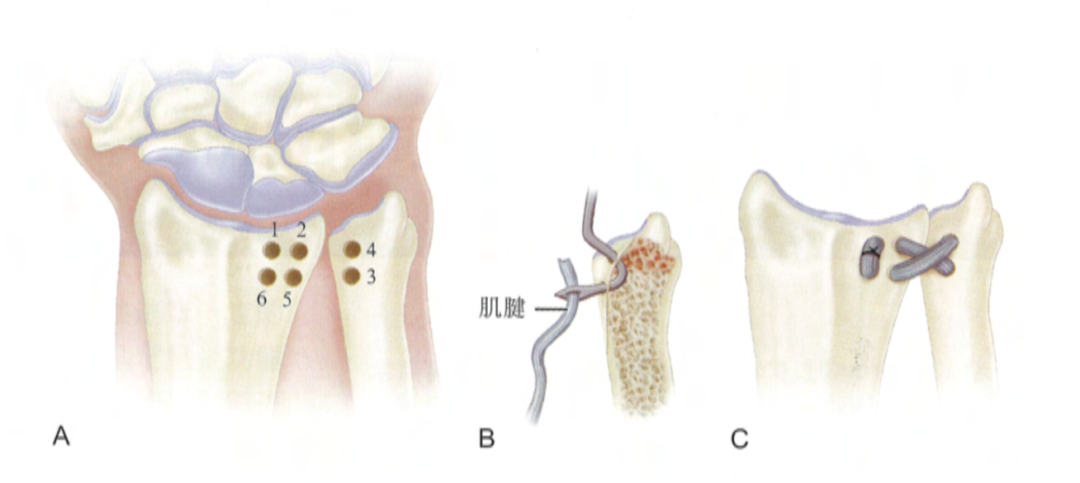
Leibolt方法。A:在尺桡骨上钻孔位置;B:穿肌腱的方法;C:关节固定后的情况
④ 下尺桡关节置换
05病例示例
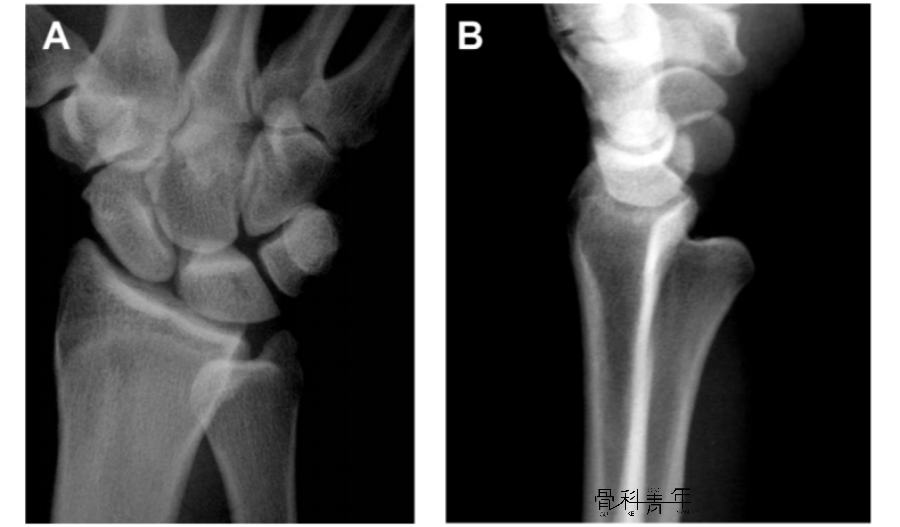
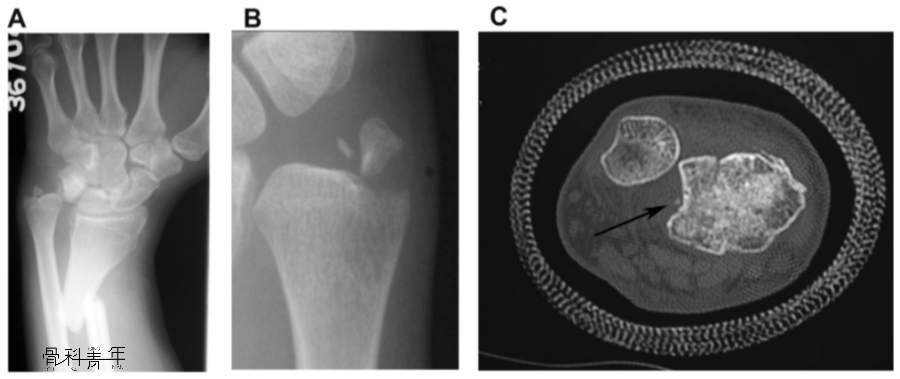
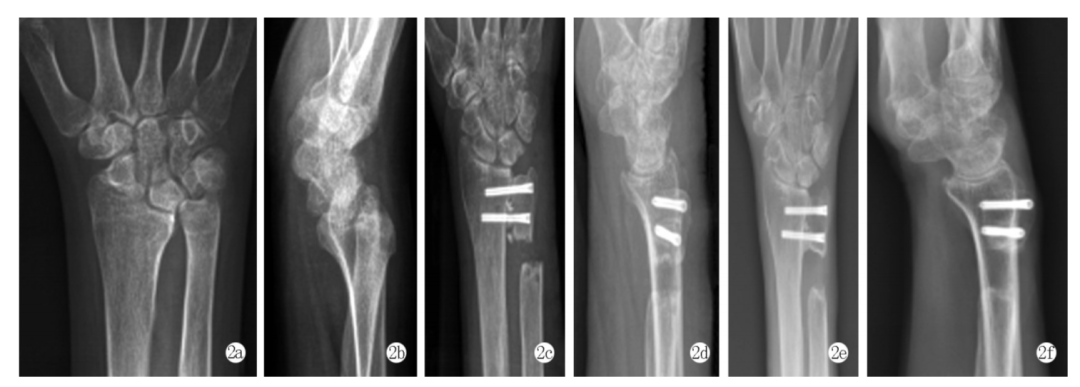
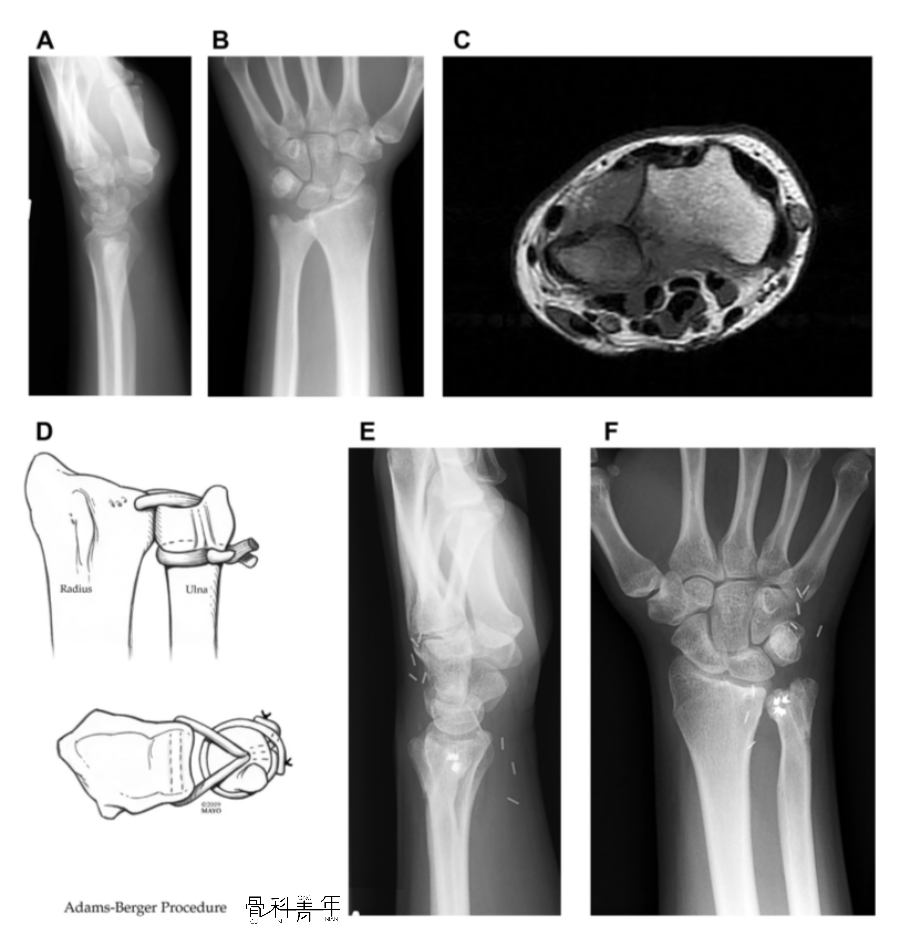
一例17岁患者,腕关节慢性疼痛3月,X线未见明显脱位(AB),MR检查提示下尺桡关节背侧脱位(C),予以下尺桡关节韧带重建(D),术后10年复查下尺桡关节位置良好,患腕无明显疼痛。
1.Poppler LH, Moran SL. Acute Distal Radioulnar Joint Instability: Evaluation and Treatment. Hand Clin. 2020 Nov;36(4):429-441.
2.房燚,赵文志,潘德悦, 等.改良Sauve-Kapandji手术治疗陈旧性下尺桡关节脱位1例[J].实用骨科杂志,2019,25(12):1147-1148.

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#桡关节#
101
#Dis#
148
#OCA#
79
#关节脱位#
82
#脱位#
90