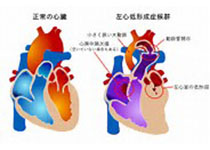
Heart:成年先天性心脏病和肺动脉高压患者心律失常状况!
2018-05-21 xing.T MedSci原创
由此可见,心律失常在PAH-CHD患者中很常见,并且与长期不良结局相关,即使在专科中心进行治疗。
大约5%-10%的先天性心脏病(CHD)患者发生肺动脉高压(PAH),这会影响预期寿命和生活质量。心律失常在这些患者中很常见,但其发生率和对结果的影响仍不确定。
近日,心脏病领域权威杂志Heart上发表了一篇研究文章,研究人员对2007至2015年期间所有在三级中心CHD相关PAH(PAH-CHD)成年患者随访新发房性或室性心律失常,并使用Cox分析评估与心律失常有关的临床变量及其与死亡率的关系。
该研究共纳入了310例患者(平均年龄为34.9±12.3岁,男性占36.8%)。大多数患者有艾森曼格综合征(58.4%),15.2%的患者既往有缺损修复,三名患者患有唐氏综合征。在基线时,14.2%的患者有心律失常史,主要是室上性心律失常(86.4%)。在中位随访6.1年期间,64名患者发生至少有一次新的心律失常发作(每年发生率为3.47%),大多数是室上性心动过速或房颤(78.1%的患者)。75.0%的病例伴有心律失常。随访期间,PAH-CHD的类型、疾病严重程度和既往心律失常标记与心律失常有关。即使在调整了人口统计学和临床变量后,心律失常也是死亡的强有力的预测因素(HR为3.41,95%CI为2.10-5.53,P<0.0001)。
由此可见,心律失常在PAH-CHD患者中很常见,并且与长期不良结局相关,即使在专科中心进行治疗。
原始出处:
Maria Drakopoulou,et al.Arrhythmias in adult patients with congenital heart disease and pulmonary arterial hypertension. Heart. 2018. http://dx.doi.org/10.1136/heartjnl-2017-312881
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#动脉高压#
41
#肺动脉高压患者#
45
学习了.谢谢作者分享!
101
学习
90
#ART#
34
#先天性#
34
#HEART#
33
肺动脉高压表面是罕见病,事实上临床上并不少见,治疗药物虽然有一些,但是整体仍然不理解,可能未来需要采用综合治疗措施。
62