Hepatology:HCV通过巨噬细胞激活肝星状细胞介导CCL5分泌
2017-03-29 MedSci MedSci原创
背景:HCV引起的慢性肝病是当前严重的健康问题,常引起纤维化/肝硬化及肝细胞癌。尽管炎症反应被认为在疾病的发生中发挥重要作用,但HCV感染期间肝脏疾病进展的具体机制尚不清除。方法:我们先前报道了包括Kuffer细胞在内的巨噬细胞暴露在HCV时,产生前炎症细胞因子。这些细胞因子可激活肝星状细胞致纤维化。在本研究中,我们研究了在HCV感染是巨噬细胞同肝星状细胞的相互作用。原代人肝星状细胞及永生的肝星状
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#分泌#
54
#肝星状细胞#
67
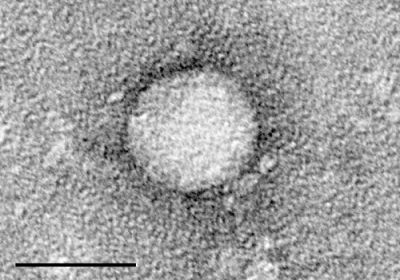
#HCV#
49
#EPA#
59
#CCL5#
54