Clin Gastroenterol H:HCV患者抗病毒治疗后肝脏硬度降低程度如何?
2017-05-08 xing.T MedSci原创
在这项系统回顾和荟萃分析中,研究人员发现根除HCV感染(SVR)可以显著降低肝脏硬度,尤其是在基础炎症水平较高的患者或服用直接抗病毒药物的患者中。几乎一半的患者治疗前被认为存在晚期肝纤维化,基于VCTE,治疗后可以达到肝脏硬度低于9.5kPa。
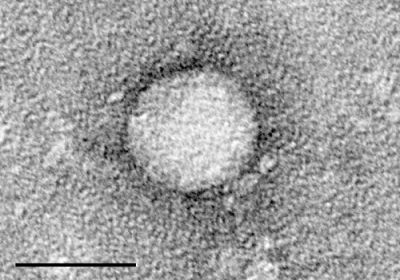
近日,消化病领域权威杂志Clinical Gastroenterology and Hepatology发表了一篇荟萃分析文章,研究人员旨在评价达到持续病毒学应答(SVR)水平的丙型肝炎病毒(HCV)感染者通过振动控制的瞬时弹性成像(VCTE)测量的肝脏硬度降低程度。
研究人员检索了截止至2016年10月的在接受抗病毒治疗(无论是直接作用的抗病毒药物或干扰素为基础的治疗)的HCV感染的成年患者进行的观察性研究或随机对照试验,患者的肝脏硬度是通过VCTE在治疗开始前和完成治疗后随访期间至少测量一次;研究还提供了达到和没有达到SVR水平的患者肝脏硬度的均值或中位数。研究人员确定了24项研究,并采用随机效应荟萃分析估计了达到和没有达到SVR水平患者的加权平均差(和95%CI)。
在达到了SVR的患者中,治疗结束后肝脏硬度下降了2.4kPa(95%CI:-1.7至-3),治疗后1-6个月为3.1kPa(95%CI:-1.6至-4.7),治疗6-12个月为3.2kPa(90%可信区间为-2.6和-3.9),或治疗后超过12个月为4.1kPa(95%可信区间为-3.3至-4.9)(平均减少了28.2%;四分位间距范围为21.8-34.8%)。与此相反,在没有达到SVR水平的患者中肝脏硬度没有显著变化(治疗后6-12个月,减少了0.6kPa;95%可信区间为-1.7至0.5)。肝脏硬度的降低程度在采用直接作用的抗病毒药物治疗的患者中更明显,相比于干扰素治疗的患者(降低4.5kPa vs. 降低2.6 kPa;P=0.03)、基础肝硬化患者(降低5.1kPa vs. 无肝硬化患者降低2.8kPa;P=0.02)或治疗前谷丙转氨酶水平升高的患者(P<0.01)。在基础肝脏硬度大于9.5kPa的患者中,47%(95%可信区间为27%-68%)的患者在接受治疗后肝脏硬度小于9.5kpa。
在这项系统回顾和荟萃分析中,研究人员发现根除HCV感染(SVR)可以显著降低肝脏硬度,尤其是在基础炎症水平较高的患者或服用直接抗病毒药物的患者中。几乎一半的患者治疗前被认为存在晚期肝纤维化,基于VCTE,治疗后可以达到肝脏硬度低于9.5kPa。
原始出处:
Siddharth Singh,et al. Magnitude and Kinetics of Decrease in Liver Stiffness After Anti-viral Therapy in Patients With Chronic Hepatitis C: A Systematic Review and Meta-analysis. Clinical gastroenterology and hepatology 2017. http://www.cghjournal.org/article/S1542-3565(17)30532-3/fulltext
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#肝脏硬度#
126
#GAS#
104
#AST#
108
#Gastroenterol#
64
#HCV#
82
#抗病毒#
93
#抗病毒治疗#
63
看过了,看过了
100
根除hcv,降低肝硬化的程度,但是肝功能逆转的了么?
0
学习啦谢谢分享
145