Nature:新突破:胰腺癌治疗新方法——羟化氯喹+化疗
2020-04-26 佚名 转化医学网
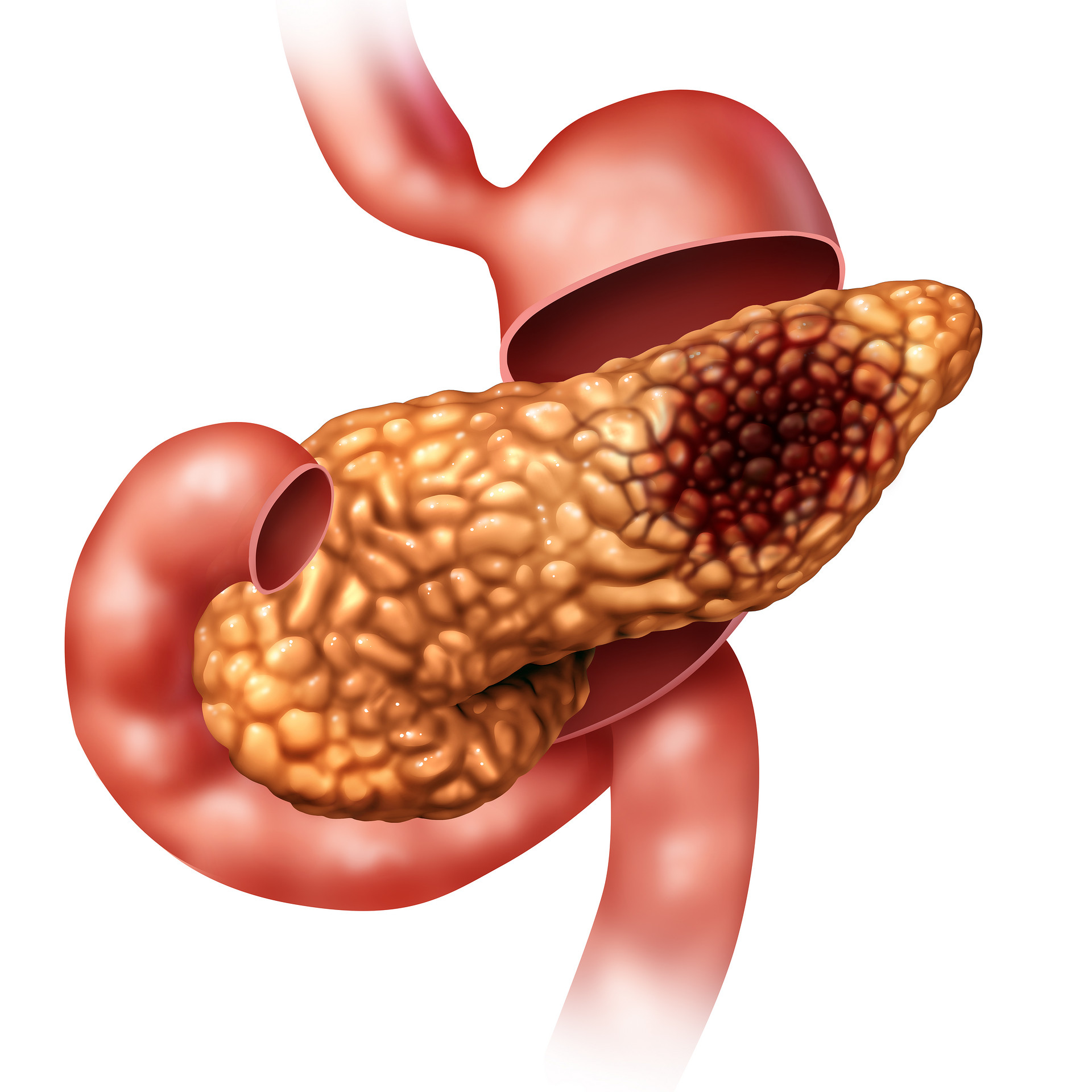
胰腺癌是一种恶性程度很高,诊断和治疗都很困难的消化道恶性肿瘤,约90%为起源于胰管上皮的导管腺癌。其发病率和死亡率近年来明显上升。胰腺癌有病程短、病情发展快和迅速恶化等特点,是预后最差的恶性肿瘤之一。
胰腺癌是一种恶性程度很高,诊断和治疗都很困难的消化道恶性肿瘤,约90%为起源于胰管上皮的导管腺癌。其发病率和死亡率近年来明显上升。胰腺癌有病程短、病情发展快和迅速恶化等特点,是预后最差的恶性肿瘤之一。最近对胰腺癌的研究有了新突破。
纽约大学格罗斯曼医学院(NYU Grossman School of Medicine)的一项新研究发现,胰腺癌细胞使用一种正常的废物清除过程去隐藏它们表面的标签,不让免疫系统摧毁它们,这项研究在4月22日在线发表在《自然》上。这项研究结果有助于回答了一个长期存在的问题:为什么胰腺癌细胞抵制免疫治疗呢?免疫治疗是使用身体自身的免疫防御去攻击癌细胞。
这项研究关注于主要的组织相容性复合体1类(MHC-1),MHC-1是一组在细胞表面呈现的特定的蛋白质片段。免疫系统的T细胞会忽略那些带有MHC-1标记的细胞,MHC-1细胞对每个人的细胞都呈现“自我”标记,但它们会识别和攻击带有奇怪标记的细胞,比如那些感染了病毒的细胞,在某些情况下,还会攻击已经癌变的细胞。
由纽约大学兰贡分校放射肿瘤学系和珀尔穆特癌症中心以及加州大学旧金山分校的研究人员主导的这项新研究,发现在在胰腺癌中,MHC-I被拖入癌细胞内称为囊泡的隔间,并被自噬降解,回收受损细胞组件的正常过程。研究人员表示,通过去除MHC-I标记,自噬使癌细胞能够避开免疫系统的注意,并使它们对免疫疗法产生抵抗。
这项新研究表明,在胰腺癌细胞中,MHC-1进入隔间(也称囊泡),在癌细胞里面,被自我吞噬降解,一个正常的过程会再循环损伤的细胞组分。通过移除MHC-1标签,自我吞噬能够让癌细胞不被免疫系统注意到,也让癌细胞对免疫治疗有了抵抗力。
该研究的资深合着者、医学博士亚力克·基梅尔曼(Alec Kimmelman)和安妮塔·斯特科勒(Anita Steckler)、纽约大学兰贡分校放射肿瘤学系的主席、教授约瑟夫·斯特科勒(Joseph Steckler)一起表示,“我们的研究表明,阻断自我吞噬,或者在基因上或者在药物上,都会增强MHC-1在胰腺癌细胞表明的表达。”
珀尔穆特癌症中心高级领导基梅尔曼博士补充说,“这一新发现的免疫逃避作用增加了越来越多的证据,支持胰腺癌或其他癌症中自我吞噬途径的靶向性。”例如,基梅尔曼博士的实验室先前的研究表明,胰腺癌细胞利用自我吞噬产生一种降解的细胞成分,作为恶性细胞生长的燃料。
胰腺导管腺癌(PDAC)是最普遍的胰腺癌类型,它是使用免疫检查点抑制剂药物治疗无效的癌症类型之一。基梅尔曼博士表示,尽管这些治疗方法失败的原因很复杂,基因改变(突变)导致肿瘤细胞表面MCH-1的缺失是一个起因,然而PDAC肿瘤并没有这些突变,表明仍有其他机制在起作用。
基梅尔曼博士和加州大学旧金山分校的资深研究合着者拉舍卡·佩雷拉(Rushika Perera)博士独立确定,MHC-1的相当一部分不再存在于胰腺癌细胞的表面,而是存在于细胞内,这两个实验室随后合作证明,一种自我吞噬蛋白(也称NBR1)附着在MHC-1上,MHC-1将其输送到自我吞噬体,然后进入溶酶体,在溶酶体中像细胞废物一样被分解了。
在患有胰腺癌的小鼠实验中表明,用基因方法或用抗疟疾药物氯喹阻断自我吞噬会导致MHC-1分子在肿瘤细胞表面的增加。众所周知,氯喹和它的衍生羟化氯喹,羟化氯喹被测试出在很可能能够治疗COVID-19,研究人员也发现,在小鼠模型中,氯喹和两种免疫检查点抑制剂的联合使用会极大提高肿瘤表达,远胜于单独的免疫治疗。
研究人员也研究了非小细胞肺癌的肿瘤细胞系,发现MHC-1也在这些肿瘤中的一部分也通过自我吞噬降解。这些研究表明,MHC-1在胰腺癌细胞内化引起的免疫治疗抵抗力可能在其他癌症类型中起作用。
对胰腺癌患者的临床测试已经表明,羟化氯喹与标准的化学治疗结合会增加患者对化学治疗的反应。新研究表明,羟化氯喹可能提高免疫治疗的效果。基梅尔曼博士警告称,虽然前景看好,但这种结合还需要进一步研究,才能进行临床测试。
共同领导研究的作者、医学博士山本圭佑(Keisuke Yamamoto)和实验室的博士后研究员基梅尔曼博士表示,“我们研究的下一步就是在患者身上测试,我们的目标就是搞清楚如何使用羟化氯喹、免疫治疗对化学治疗进行排序,去识别可能反应的患者亚组织的标记物。
参考文献:
Keisuke Yamamoto,et al.Autophagy promotes immune evasion of pancreatic cancer by degrading MHC-I.Nature (2020).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#新方法#
56
#治疗新方法#
60
#胰腺癌#羟氯喹增敏,氯沙坦增效
210
#新突破#
59
#Nat#
52
了解一下
125
好
125