产前超声诊断妊娠子宫圆韧带静脉曲张2例
2020-05-12 张元吉 卢峻 吴淮宇 临床超声医学杂志
病例1,患者30岁,孕1产0,因孕32周发现左腹股沟区包块就诊。体格检查:左腹股沟区见一包块,质软,无触痛,站立时缓慢增大,临床考虑左侧腹股沟疝。超声检查:子宫圆韧带走行区域见蔓状静脉丛,其内可见多个
病例1,患者30岁,孕1产0,因孕32周发现左腹股沟区包块就诊。体格检查:左腹股沟区见一包块,质软,无触痛,站立时缓慢增大,临床考虑左侧腹股沟疝。超声检查:子宫圆韧带走行区域见蔓状静脉丛,其内可见多个蚓状无回声区,范围约37 mm×18 mm;CDFI于其内可探及红蓝相间血流信号(图1)。
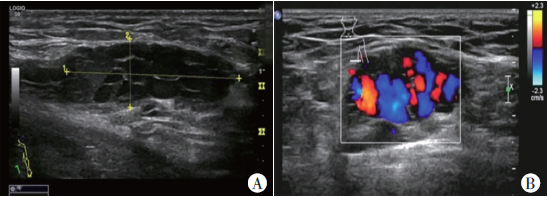
图1 左侧妊娠子宫圆韧带静脉曲张声像图。A:左侧腹股沟区可见多个蚓状无回声区;B:CDFI示其内可探及丰富红蓝相间血流信号
超声提示:子宫圆韧带走行区域静脉曲张。孕妇妊娠期未治疗,产后11个月余复查超声未见子宫圆韧带静脉曲张。
病例2,患者30岁,孕2产1,因孕33周发现右侧腹股沟区包块就诊。体格检查:右侧腹股沟区见一包块,质地稍硬,有触痛,临床拟诊右侧腹股沟疝。超声检查:右侧腹股沟区见一大小为73 mm×16 mm异常回声,向上与子宫相连,形态不规则,边界尚清晰,其内回声不均匀,大部分呈无回声,并可见条索状强回声及低回声区,挤压包块不变形;CDFI示其内可探及少许血流信号,并可测得静脉血流频谱(图2)。
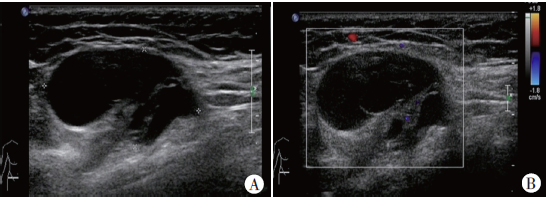
图2 右侧妊娠子宫圆韧带静脉曲张并血栓形成声像图。A:右侧腹股沟区混合性异常回声,加压探头不变扁;B:CDFI示其内可探及少许血流信号
超声提示:右侧腹股沟区所见异常声像,考虑子宫圆韧带静脉曲张伴血栓可能。孕妇妊娠期未治疗,产后1年余复查超声显示右侧腹股沟区未见异常声像。
讨论
子宫圆韧带是固定子宫的主要韧带,呈圆索状,内包绕动脉、静脉、淋巴管及神经走行。子宫圆韧带静脉曲张是指子宫圆韧带伴行的静脉丛迂曲扩张,是一种发生于女性妊娠期的良性疾病,与男性精索静脉曲张性质相似。其可发生于子宫圆韧带走行的任何区段,包括子宫肌层、腹股沟管及大阴唇,多见于妊娠期妇女。本病临床主要表现为腹股沟区包块,可有压痛,在腹压增加或改变体位时增大;多见于左侧,这主要是由于圆韧带静脉丛延续为卵巢静脉,左侧卵巢静脉以较垂直的角度汇入左肾静脉。
该病预后较好,多数病例于产后自行消失,并发症主要包括静脉曲张破裂出血和血栓形成等,本病即便出现并发症,仍可选择保守治疗。本文报道的2例病例中,妊娠期均未予治疗,产后静脉曲张亦自动消失,与文献报道一致。本病主要与以下疾病进行鉴别:①腹股沟疝:尤其是可复性疝,与子宫圆韧带静脉曲张临床表现相似,易误诊,腹股沟疝超声见肠系膜脂肪稍高回声并可见肠蠕动,血流特点为黏膜内的点状血流信号;②与其他腹股沟区疾病:腹股沟区海绵状血管瘤、腹股沟管囊肿及子宫圆韧带囊肿等鉴别,这些病变均不与子宫相连,结合病史及血流特点即可鉴别。超声在发现并诊断子宫圆韧带静脉曲张方面具有较高的价值,可明确诊断,避免患者进行不必要的临床干预。
原始出处:
张元吉,卢峻,吴淮宇,熊奕.产前超声诊断妊娠子宫圆韧带静脉曲张2例[J].临床超声医学杂志,2019(02):153.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言


















#产前超声#
87
#静脉#
65
#产前#
93
#韧带#
94
#超声诊断#
97
#超声诊断#
79