步态冻结(FOG)是影响许多帕金森病(PD)患者的一种衰弱症状,被定义为 "尽管有行走的意图,但脚步短暂的、发作性的缺失或明显减少。这导致跌倒的风险增加,并对身体和精神健康相关的生活质量产生重大影响。众所周知,由于对多巴胺替代疗法的反应不同,以及左旋多巴随着时间的推移对FOG的潜在负面影响,FOG的治疗具有挑战性。此外,康复治疗的效果是短期的,只有在FOG仍然轻微时才有可能。鉴于这些挑战,FOG发病的标志物对于筛查FOG转换和预先提供治疗至关重要。
图1 论文标题图
到目前为止,各种研究已经调查了转化为FOG的临床风险因素。然而,只有一项研究调查了转换的神经标志物,并发现纹状体多巴胺能缺陷对这种转换的临床预测模型有额外贡献。
由于证据有限,有必要对转换的神经标志物进行调查,以达到额外的预测目的,并帮助解释导致FOG发病的难以捉摸的机制。
虽然FOG可能标志着皮层-基底节-丘脑-皮层平行回路的暂时性信息处理障碍,但这些暂时性事件在诱发和解释方面具有挑战性,因此作为预测性标记的适用性较差。
然而,这些回路中的节点的补偿性或适应性结构改变更持久,因此更容易捕捉到作为PD中FOG的可能预测标志物。
最近对PD和FOG患者结构改变的横断面调查的系统回顾显示,广泛的皮质和皮质下灰质萎缩,以及FOG严重程度与萎缩之间的关联,表明灰质形态可能是FOG发病和进展的有用标记。
此外,当中枢或外周起源的PD病理进入大脑时,皮质下结构受影响较早,也许是FOG发病的早期标志物。然而,目前还缺乏对这一假设的前瞻性评估。
因此,在这项纵向研究中,比利时鲁汶大学的Nicholas D’Cruz等人, 利用磁共振成像(MRI)调查了与FOG相关的关键皮层下结构的形态学变化。他们比较了研究开始时和两年内没有出现或在研究期间出现FOG的参与者(非转换者)与那些在研究开始时出现FOG(冷冻者)或在研究期间出现FOG的参与者(转换者)之间的局部和整体体积差异。
根据以前的横断面工作,核心假设:患有或即将发生FOG的人,与非转换者相比,在脑干、丘脑和/或尾状腺会出现局部或整体体积下降,这可能作为FOG转换的神经标志物。
然后,他们评估了研究开始时的结构性标志物对两年内转换为FOG的预测程度,并探讨了它们的行为关联和潜在的核下容积和功能关联。
最后,利用帕金森病进展标志物倡议(PPMI)队列的数据对这些标志物进行了初步验证。
在研究开始时,他们发现FOG者(N = 12)和在研究过程中出现FOG的人(转换者)(N = 9), 与没有转换者(非转换者)(N = 36)相比,显示出双边丘脑增加。
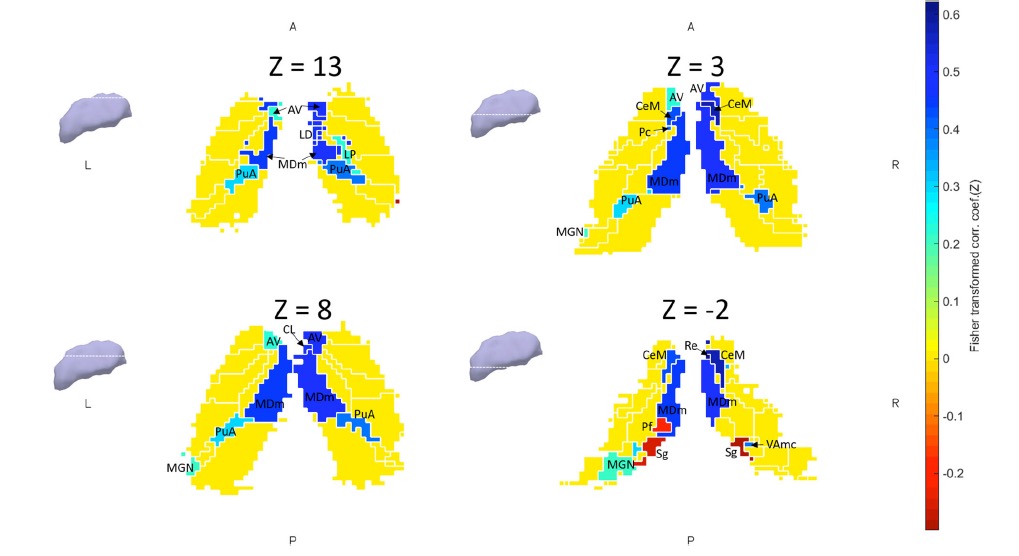
图2 丘脑形态学变化示意图
纵向来看,转换者(N = 7)与非转换者(N = 36)相比,也显示出左侧丘脑的局部膨胀。一个包括性别、每日左旋多巴等效剂量和丘脑局部膨胀的模型可以很准确地预测转化率(AUC:0.87,敏感性:88.9%,特异性:77.8%)。
探索性分析显示,局部丘脑充气与较大的丘脑内侧亚核体积和更好的认知表现有关。静止状态分析进一步显示,转换者在转换前与边缘区和认知区有更强的丘脑-皮质耦合,而在两年内耦合明显减少。
最后,使用PPMI队列的验证表明,FOG特定的丘脑局部体积的非线性演变。
该研究的重要意义在于发现了:丘脑的形态变化或可作为FOG的标志物,这可能会促进早期干预和改善PD患者的行动能力。
原文出处:
D’Cruz N, Vervoort G, Chalavi S, Dijkstra BW, Gilat M, Nieuwboer A. Thalamic morphology predicts the onset of freezing of gait in Parkinson’s disease. npj Parkinsons Dis. 2021;7(1):20. doi:10.1038/s41531-021-00163-0
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言


















#冻结步态#
83
#Dis#
95
#步态#
112
#丘脑#
104
#丘脑#
79