J Clin Oncol:新辅助治疗可提高早期直肠癌患者的肛门保留率
2022-08-20 MedSci原创 MedSci原创
三个月的诱导化疗有望成功降低相当一部分早期直肠癌患者的肿瘤临床分期,从而可采取耐受性良好的器官保留手术
早期 I/IIA 期直肠癌的器官保留治疗旨在避免与全直肠系膜切除(TME)相关的功能障碍或永久性造口术。该研究旨在确定接受新辅助化疗和经肛门切除手术 (TES) 治疗的早期直肠癌患者的预后和器官保留率。
这是一项 2 期临床试验,纳入了符合内镜切除术且接受 3 个月化疗的临床 T1-T3abN0 期低位或中位直肠腺癌患者。有缓解证据的人在 2-6 周后进行经肛门内窥镜手术。主要终点是方案规定的器官保留率,定义为肿瘤降期至 ypT0/T1N0/X 期且避免了根治性手术的患者比例。
共入组了58位患者,全部进行了化疗,其中56位进行了手术。共有33/58位患者的手术标本肿瘤降期至 ypT0/1N0/X 期,导致意向治疗方案指定的器官保留率为 57%。在根据方案要求推荐进行 TME 手术的23位剩余患者中,13位拒绝并选择进行观察,因而器官保留率为 79%。在10位进行了 TME手术的患者中,有7位没有组织病理残留病灶。
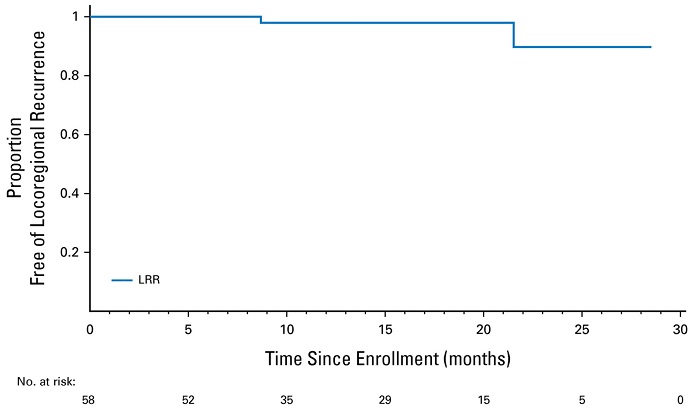
无局部复发生存率
一年无局部复发生存率是98%,两年无局部复发生存率是90%,且无远处复发或死亡病例。生活质量和直肠功能评分的变化均很小。
总之,三个月的诱导化疗有望成功降低相当一部分早期直肠癌患者的肿瘤临床分期,从而可采取耐受性良好的器官保留手术。
原始出处:
Hagen F. Kennecke, et al. Neoadjuvant Chemotherapy, Excision, and Observation for Early Rectal Cancer: The Phase II NEO Trial (CCTG CO.28) Primary End Point Results. Journal of Clinical Oncology. August 18, 2022. https://ascopubs.org/doi/full/10.1200/JCO.22.00184
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#新辅助#
115
#肛门#
99
#Oncol#
117
#直肠癌#
98